Chemical Exposure in Firefighting: The Enemy Within
FEATURES
HEALTH
The call came in at approximately 3 A M on March 16, 1981. When the engine company and hazardous materials squad arrived at the scene, they found a 2,000gallon chemical spill on Interstate 5 covering the parking lot of a local truckstop. Whatever it was* had eaten its way through the bottom of an aluminum tanker truck. Wearing self-contained breathing apparatus (SCBA), the firefighters erected barricades and quickly evacuated pedestrians.
The crew spent hours containing the chemical while constantly monitoring the spill with an explosimeter. The vapors were dense and bathed the firefighters and police officers (who were not wearing SCBA).
After being relieved from duty, Firefighter David Werner returned to the “safe zone” and removed his protective gear. In 1981, there were no rules or procedures about decontamination to follow. So Werner, like many others, still wearing his vapor-coated turnout suit, removed his SCBA to breathe in “fresh” air. An hour later he was in the hospital.
Captain Mel Howard, who has been a firefighter for over 30 years, said that he didn’t experience any acute exposure during that or any other chemical emergency. “There was never any one incident in which exposure to chemicals on the job left me debilitated.”
However, Captain Howard suffered from chronic low-level toxic exposure. He experienced blind-
*Th© chemical was later identified as 1,2 dichloropropane which is known to react violently with aluminum. ing headaches for no reason at all; he would even wake from a deep sleep with them. He had terrible skin rashes on his legs, and he would feel extreme fatigue in the early morning.
After reading a report by Gary Girod, assistant fire marshal in the Hazardous Materials Section of the Bureau of Fire Prevention in Ventura, CA, that described the symptoms of firefighters exposed to toxics, Howard became concerned.
“I have spent more than 30 years in the fire department,” explains Howard. “I have been exposed to just about every chemical industrially available and commercially shipped. I became concerned that I would not be healthy for my retirement years.”
GROPING FOR SOLUTIONS
For David Werner, the next five years were ones of suffering and frustration. He left the hospital feeling only slightly ill; throat irritation, a mild cough, fatigue, and some lack of coordination and concentration.
As time went on, however, these symptoms began to get worse. His cough became much more severe. He would have coughing fits to the point of straining chest muscles. His head constantly pounded and his ears buzzed for over four years. And he got sick. He was ill from colds more that first year following the chemical spill incident than he was any other year of his life. Further, when he would cut or bruise, he would not heal as quickly. The rashes he got seemed to appear more frequently and would scar as they healed.
“It just seemed as though my whole immune system was breaking down and going haywire,” states Werner. “Gradually it affected my entire body; every joint felt inflamed.”
According to Werner, his hands and feet often went numb and when he bent his arm at the elbow, he would lose the feeling in his arm completely. He would fatigue easily and regularly have to nap during the day.
“Basically, all of my free time was spent sleeping,” Werner explains. “If I didn’t sleep, I would walk around like I was drugged.”
Werner also suffered through many cognitive problems. He would forget integral pieces of information like hydraulic pressures and street locations that are critical to know during an emergency.
“There were times when I would even forget my own telephone number,” reports Werner. “Once I even forgot how to tell time. Quite often I couldn’t remember what I was talking about or where I was in a game. My concentration was crippled. My mind would wander aimlessly between spurts of attention.”

Werner also suffered periods of extreme irritability. Although he describes himself as a “kickback kind of guy,” after the accident he found that there were many times when he would just jump all over people.
“It didn’t take much to set me off,” he explains. “There was a tremendous amount of stress, which, when added to the stress of the job, was insurmountable.”
Werner went from specialist to specialist but received no relief. Most could find nothing wrong with him and some even attributed his problems to psychosomatic illness.
“It wasn’t that the doctors weren’t qualified,” states Werner. “All of them were experts in their fields. The problem was that they did not have all of the information on the chemicals or treatment for exposure to properly evaluate my situation. That was the most frustrating thing: knowing I was sick and knowing how and when it happened, yet having the experts tell me that I was not sick because nothing was confirmed by their tests.”
Frustrated with the physicians, Werner began researching the subject of chemical toxicity. He discovered that 1,2 dichloropropane was not the only substance to which he had been exposed. He had been exposed to a number of reaction by-products while standing in the “safe zone” which complicated the situation.
“When a doctor would treat me, he would look in his books for the proper course of action for exposure to 1,2 dichloropropane,” states Werner. “He would not look into the other chemicals that I was exposed to.”
“A major part of the problem is that most doctors have not been adequately educated in the diagnosis and treatment of chemical exposure cases,” says Dr. James Dahlgren, an assistant professor at UCLA and medical director of Pacific Toxicology Laboratories where human tissue samples are analyzed for chemical contamination. “Modern lab techniques allow us to pinpoint almost any kind of toxic chemical in the body. Fortunately, an increasing number of physicians now recognize the often puzzling nature of chemically related ailments and are using clinical labs as a diagnostic tool.”
Unlike Werner, Captain Howard’s symptoms developed over a period of many years and illustrate how truly insidious is the problem of chemical buildup in the body. Whereas Werner was chemically galvanized into defending his health against one unmistakable opponent, Howard was slowly and covertly ground into a state of unrelenting malaise by an invisible enemy.
“My legs would feel as sore as if I had just run a marathon in my sleep,” states Howard. “For periods of one to two months at a clip, my legs would ache when I awoke; they were just beat. There were also times when I would have temper flare-ups over little things that shouldn’t have bothered me. All of a sudden, I would become very irrational and be tremendously irritated; and, just as quickly, it would pass and I would be very embarrassed.”
BIO-ACCUMULATION
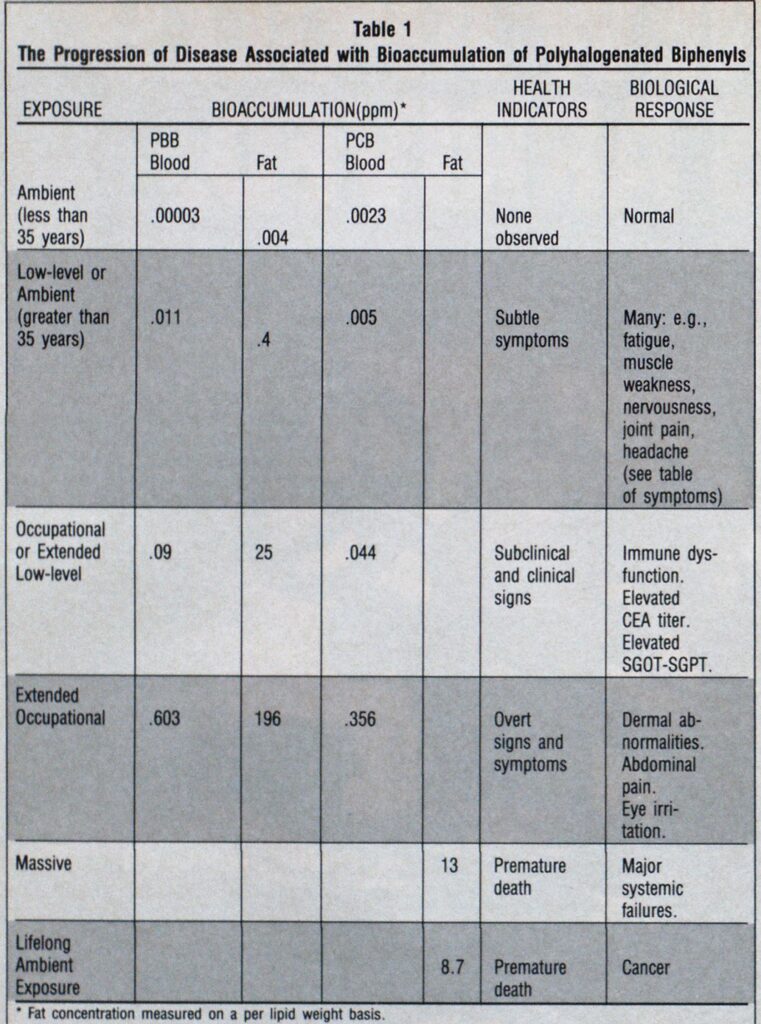
Perhaps the greatest hazard posed by many of the toxic chemicals which firefighters face is that they accumulate in the body. One major storage site is the fat, a component of most bodily organs and systems, including the brain and nervous system. This storage is caused by the body’s inability to process these chemicals to a point where it can excrete them. Scientists term this bio-accumulation.
However, whenever any stress is applied to the body, these chemicals are released into the bloodstream and can circulate to virtually any organ, only to return later to the fat. The stresses that induce this on-going circulation of toxins are common, everyday occurrences. Fasting (even when one merely sleeps), heat exposure, dieting, strenuous exercise, and medical conditions such as pregnancy and illness are all examples of stresses which mobilize these toxins. Thus, it is at those times on the job when a firefighter least wants toxic chemicals impairing his or her performance that they are most likely to be in circulation.
The damage that can be caused by these chemicals is far-reaching. When foreign substances enter the body, each cell or each organ must “take time out” and expend energy to process the toxin to every extent that is possible. Then, because these molecules are resistant to decomposition, the cells and organs must also expend energy “shipping” these molecules to the liver and kidneys, which tends to wear them down. The process has also been shown to cause diseases such as cirrhosis of the liver and damage to the kidneys.
A second adverse effect is carcinogenicity. Although there is much to learn about the mechanisms involved, there is a growing body of evidence linking many toxic chemicals with a weakening of the human immune system. The immune system protects us from a variety of diseases, including cancer. Thus, toxic substances may predispose us, through compromising the immune system, to contracting a variety of illnesses.
Toxic chemicals also bring about a physiological dilemma that might be termed “bioconfusion.”
“When a foreign chemical is thrust upon it, the body may have difficulty differentiating the compound from substances it needs,” explains Dr. William Marcus, chief toxicologist for the Environmental Protection Agency’s Office of Drinking Water. “For example, the chemical structure of the indispensible hormone thyroxin is strikingly similar to that of DDT (dichloro-diphenyl-trichloro-ethane), PCB (polychlorinated biphenyls), and dioxin.”

To address the problem of chemical storage, researchers with the Foundation for Advancements in Science and Education years ago began to study a technique designed to reduce bodily stores of contaminants. The detoxification method, developed by the late American researcher L. Ron Hubbard, integrates aerobic exercise and closely monitored sessions in a well ventilated sauna with polyunsaturated oil and vitamin and mineral supplements to maintain body chemistry. Exercise, heat, and niacin (vitamin B3) mobilize the fat in the body, including the toxins stored therein. Once in the bloodstream, the toxins are channeled into the sweat and sebum (body oil) and secreted. The oil supplements also enhance excretion through the feces. Treatment usually takes about two to three weeks on a schedule of two and a half to five hours daily.
Studies of the technique were conducted using Michigan farmers exposed to PBB (polybrominated biphenyls), a highly persistent fire retardant chemical which accidentally made its way into the Michigan food chain in 1973. This work, published by the Royal Swedish Academy of Sciences, reports a reduction of 21.3% on the average for the 16 chemicals (PBB, PCB, and various pesticides) tested post-treatment; and, a reduction of 42.4% four months later. Similar results were found in a controlled study of electrical workers exposed to PCB which was published by the International Agency for Research on Cancer (Scientific Publications Series, Volume 77, Oxford University Press).
CLINICS OFFER TREATMENT
The detoxification technique was adopted in 1982 by physicians at the HealthMed Clinic, a medical facility with clinics in Los Angeles and Sacramento, CA, which has treated over 1,200 persons using the regimen, including a number of firefighters.
Firefighter Werner entered the treatment program nearly five years after his initial exposure. While going through the treatment, he experienced several manifestations of his exposure-related problems. His headaches and foot pains would appear and disappear while in the sauna. His skin rashes and assorted pains and ailments all came back. And just as mysteriously as they would appear, they would disappear.
HealthMed’s Los Angeles Medical Director, Dr. Megan Shields, explains this phenomenon: “As stored substances move into circulation and are eliminated from the body, people commonly re-experience symptoms associated with the chemical exposure. This discomfort seems to signal a marked change in health status and is usually followed by the rapid diminution or, in some cases, the complete disappearance of the symptoms.”
Gradually, Werner’s health improved and by the end of the treatment period (27 days for Werner) most of his symptoms were either entirely gone or greatly improved.
“After the program, I felt fantastic,” declares Werner. “I feel 100% better. The thing that I notice the most is that I do not feel that I am constantly under the influence of toxins in my body. I feel more alert and aware of my surroundings.”

Captain Howard’s experience was very similar. While in the sauna he experienced severe headaches which would go away while he was still in the sauna. Another manifestation was skin rashes. His thighs were covered from back to front with this rash.
“They really came out while I was in the sauna,” states Howard. “I would get huge welts which were extremely painful. A week later they would be gone. This problem is now much, much lighter, not like it was before.”
After completing the program, Howard also stated that he was less fatigued and irritable. “I have a general feeling of well being, and I feel more alert and clearheaded.”
Chief Girod, whose report prompted Howard to take action and who lectures widely on hazardous materials in firefighting suggests that “Firefighters at risk of high exposure to toxic materials should be periodically tested so that we can adequately monitor their intake and accumulation of chemicals. Where levels are high, an effective detoxification procedure is certainly warranted.”
SUMMARY
With the increasing number of synthetics, polymers, and chemicals being incorporated into every aspect of daily life, the threat of harm to the health of the firefighter is growing. The problem is one of both acute exposures and the gradual accumulation of toxic substances throughout a career. The stories of Captain Howard and Firefighter Werner are more common than one would like to think and demonstrate well the complexity of the toxics dilemma.
“Only time will tell to what extent effective detoxification can reduce a firefighter’s chances of contracting a serious illness,” states Dr. David Root, a board certified specialist in occupational medicine and medical director of the Sacramento HealthMed Clinic. “But physicians and scientists agree that one is a lot better off without a heavy toxic body burden. Our clinical observations certainly support this, and that’s quite encouraging.”
“I have no qualms about how my case was handled by the fire department,” concludes Werner. “The administration can only go by what recognized experts recommend. The mishandling of my case is not a failure of the fire department or of the doctors. It is, instead, a complete failure of what we have as a system in the medical community to deal with chemical exposure. It is clear to me now that the time of preventative toxicology in firefighting has come.”

