By Pauline E. Leary, Brandon A. Gayle, Donald G. Gross, and Michael Frunzi
The fentanyl problem in the United States has rapidly become an epidemic, as is highlighted in these and other recent news headlines: “First responders face new dangers with use of fentanyl becoming commonplace,” “Cops fighting opioids face deadly exposure to fentanyl,” and “Fentanyl is a game-changer.” This new threat to the response community is, on some level, surprising, considering fentanyl and many of its analogues have been around and in use for more than half a century. However, the illicit drug trade has changed, and cheap and powerful forms of fentanyl have hit the streets, leaving a deadly trail.
Fentanyl is a powerful synthetic opioid that has been on the market since the 1960s and is used medically to manage acute and chronic pain including cancer pain,l pain from war injuries,2 pain during childbirth,3 and postoperative pain.4 It has a potency 100 times greater than morphine. Fentanyl pharmaceutical products are currently available in many dosage forms including oral transmucosal lozenges (“lollipops”), transdermal patches, nasal sprays, and injectable formulations.5 As with other opioids, abuse of fentanyl has been documented for decades.6-7 It is abused for its intense euphoric effects and can serve as a direct substitute for heroin in opioid-dependent individuals. (5)
Aside from an outbreak of nonpharmaceutical (illegally manufactured) fentanyl-related deaths between 2005 and 2007, abuse of fentanyl has primarily been caused by the diversion of legally manufactured dosage forms of fentanyl including fentanyl lollipops, transdermal patches, and injectables. (5) These legally manufactured dosage forms contain fentanyl but in therapeutic doses. The presence of pure fentanyl manufactured outside of the United States and imported illegally by drug smugglers from places like China and Mexico, however, has increased dramatically within the past few years.8 This pure fentanyl is being laced into heroin and other drugs of abuse including counterfeit prescription pills and cocaine, creating an incredibly dangerous situation for drug abusers for a number of reasons.
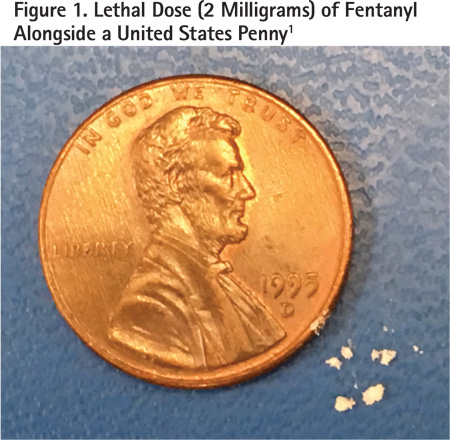
First, improper mixing of fentanyl into street samples creates lethal doses. The lethal dose of fentanyl weighs only about 2 milligrams (Figure 1), whereas the average “hit” of heroin weighs approximately 100 milligrams.9 Proper mixing of such relatively small concentrations is challenging, especially for powder samples. Improper mixing can easily result in some hits having more than 2 milligrams and others having less.
A second reason fentanyl is so dangerous to drug abusers is that if the abusers are unaware that their drug has been cut with fentanyl, they may ingest or inject their “usual” amount, causing an overdose. Reports by drug abusers indicate they frequently are not aware their typical drug of abuse has been laced with fentanyl.10
Fentanyl is a danger not only to drug abusers but also to the public at large and especially to first responders. A primary reason for this is that different types of fentanyl, known as analogues of fentanyl, may be tens to hundreds of times more potent than fentanyl. This potency is quite remarkable. When some of these analogues are encountered on scene, it is not even necessary for a first responder to touch a sample to be exposed to a lethal dose of the drug: Simple ingestion of airborne particles can occur. Exposure to small quantities can cause serious negative health effects.11 Fentanyl can rapidly suppress respiration and cause death more quickly than other opioids.12
Fentanyl Analogues: What Is the Big Deal?
Analogues are similar, though not identical, to each other. Many drugs have analogues. In fact, pharmaceutical companies routinely attempt to synthesize and develop analogues. Analogues may be exploited during drug development for a variety of reasons including development of the best possible drug candidates to bring to the market, as well as intellectual-property-rights advantages such as extension of patent protection.
Analogues are also commonly encountered in the illegal drug trade. Designer and other drugs that are slightly different from “controlled” drugs are intended to circumvent the law. This works because if the new drug being sold on the black market is different from the controlled drug (even just slightly), it may not be illegal. There are laws in place that, although they are sometimes difficult to practically apply, attempt to address the abuse of analogues of controlled substances.
In accordance with 21 USC § 813 (2011), analogues of some controlled substances, to the extent intended for human consumption, are treated for the purposes of any federal law as tightly controlled substances. Fentanyl analogues, though, have been shown to be especially dangerous because many can be significantly more potent than fentanyl. This is important considering that fentanyl, itself, is quite potent. As an example, carfentanil is reported to be 100 times more potent than fentanyl (10,000 times more potent than morphine). (8) Ingestion of microscopic amounts (20 micrograms) of this fentanyl analogue may be fatal. Remarkably, carfentanil has been cut into street samples in a number of states including Maryland,13 Pennsylvania,14 and Ohio.15
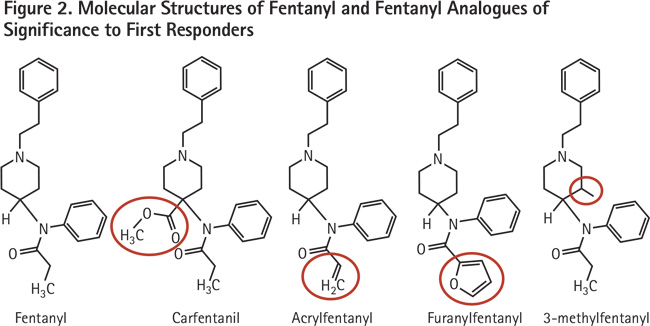
In an attempt to help pictorially describe analogues, Figure 2 shows the chemical structures of just a few of the analogues of fentanyl that are of importance to first responders. Note that the molecular structure of each of these substances is quite similar to that of fentanyl. The differences among each analogue, compared with fentanyl, is highlighted in red. These seemingly small differences in chemical structure are responsible for the sometimes remarkable differences in potency.
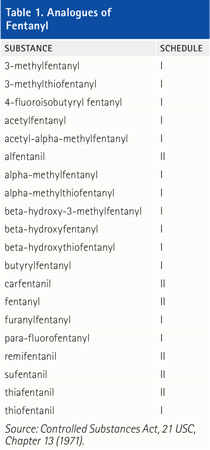
There are many analogues of fentanyl, and it is possible more may be synthesized in the future. As of June 13, 2017, 20 fentanyl analogues (including fentanyl) were listed as controlled substances under the Controlled Substances Act, 21 USC, Chapter 13 (1971). These 20 analogues are detailed in Table 1. Note that these analogues are listed as either Schedule-I or Schedule-II drugs. Schedule-I drugs have no currently accepted medical use in the United States, a lack of accepted safety for use under medical supervision, and a high potential for abuse. Schedule-II drugs have an accepted medical use and a high potential for abuse, which may lead to severe psychological or physical dependence.16
Sometime in July 2017, a 21st fentanyl analogue, acrylfentanyl, is expected to be temporarily added to Schedule I. The Drug Enforcement Administration has received reports of at least 83 confirmed fatalities associated with acrylfentanyl. These deaths occurred as early as September 2016 in Ohio, Illinois, Maryland, Pennsylvania, and New Jersey.17
How Did We Get Here?
The New York Times reports that the presence of fentanyl in seized drug samples in the United States more than doubled between 2015 and 2016 to more than 30,000. (15) This statistic itself is staggering, but it is even more alarming considering the presence of fentanyl in seized drug samples as recently as 2013 was only 978.18 Overdose deaths have also increased to a significant level. Although the number of overdose deaths for 2016 won’t be finalized until the end of 2017, it is expected that this number rose from 52,404 in 2015 to at least 59,000 (and possibly as high as 65,000) based on preliminary data analysis, the largest annual jump ever recorded in the United States. Even the low end of this range is higher than the peak number of deaths recorded in the United States in any single year because of guns (approximately 40,000 deaths in 1993), car crashes (just below 55,000 deaths in 1972), and human immunodeficiency virus (HIV) (just above 45,000 in 1995). (15)
There appear to be many factors that have contributed to this current fentanyl crisis. An increase in the number of prescriptions written and dispensed for opioid analgesics19 is likely one. In the United States, use of oral opioid analgesics has been associated with increasing rates of addiction, abuse, and diversion.20 It is also likely that fentanyl’s potency is a contributing factor, especially to the number of overdose deaths. (15) Only small amounts of the drug are needed to create a high. As a result, fentanyl and its analogues are laced into heroin with or without the knowledge of the user.21 In these situations, lethal dosing may easily occur.
It is also likely economics play a factor. The financial rewards of using fentanyl are enormous for drug dealers. One kilogram of fentanyl costs approximately $4,000 to buy from China and yields profits of $1.6 million on the streets. By contrast, one kilogram of heroin costs approximately $6,000 but is worth only a few hundred thousand dollars.22
Another potential factor is the introduction to the market of an abuse-deterrent formulation of OxyContin®. This formulation was initially introduced as a response to a rising opioid-abuse problem. OxyContin is a time-released dosage form of oxycodone HCl that has been blamed by some for the rising opioid-abuse problem in the United States.23 After the introduction of this drug to the market, some drug abusers recognized that the tablets could be crushed and then injected or snorted.24 Crushing the tablet degraded the time-release properties of the tablet, which liberated the relatively large amounts of the oxycodone HCl. The large amounts of oxycodone HCl, which were intended to be released slowly and in smaller amounts over time, created an intense high when abused in this manner.
It is now reported that an abuse-deterrent formulation of OxyContin, introduced to the market in August 2010, has shifted the abuse pattern from OxyContin to other drugs. Researchers reported a significant decrease in the number of respondents claiming the use of OxyContin as a primary drug of abuse than before the release of the abuse-deterrent formulation less than two years earlier. These researchers also cite a slight increase in the use of hydrocodone and other oxycodone agents. However, for other opioids, including high-potency fentanyl and hydromorphone, selection rose markedly. Of all opioids used to “get high in the past 30 days at least once,” OxyContin fell from 47 percent of respondents to 30 percent, whereas heroin use nearly doubled.25 Heroin is frequently tainted with fentanyl.
What Does This Mean for First Responders at the Scene?
The extremely high potency of some of the analogues of fentanyl creates a high level of potential danger for first responders and law enforcement personnel. These public servants routinely encounter powders or pills and attempt to presumptively identify these substances in the field. Historically, the potential for lethal exposure to dangerous drugs was quite low. The use of the proper level of personal protective equipment (PPE) worked well because it protected against most suspected threats, but it did not significantly encumber the responder. However, some of the analogues of fentanyl are very potent, and proper PPE can be both difficult to work in and very expensive.
The response community is struggling with recommendations on how to address samples of suspected fentanyl, especially its potent analogues. Although some guidance documents have been released, (11)26-27 no universal approach to dealing with the specific challenges associated with fentanyl compounds has been adopted by the emergency response community. It is likely, especially considering a recently published position statement of the American College of Medical Toxicology and American Academy of Clinical Toxicology,28 that when trained responders using proper PPE respond to a fentanyl scene, the risk of clinically significant exposure to fentanyl and its analogues is low. Therefore, there are some important points that responders should consider when arriving on scene to ensure their safety and the safety of others at the scene.
It is critical that responders are aware of the types of scenes at which they are arriving and when fentanyl or its derivatives may be encountered. Responses to drug overdoses should always raise a red flag, as overdose situations may occur when heroin or other opioids are cut with fentanyl. It is also important to be especially vigilant when powder samples are present. Airborne particles of fentanyl powder, especially some of its potent analogues, can be very dangerous. Clandestine laboratories should also be considered prime suspects for the presence of fentanyl compounds. For these situations, it is critical that proper PPE be selected for mitigation of the scene and that proper decontamination procedures be followed after the incident.
Detection Systems
Deployment of the appropriate detection and identification equipment at scenes where the presence of fentanyl is suspected is important. Specifically, consider the limitation of each piece of equipment or test performed and also the level of PPE required to safely perform the required testing. Methods and equipment frequently used at these types of scenes including color tests, ion mobility systems, infrared systems, and Raman systems.
Although color tests are subjective, they can be useful in some instances to screen drug substances and offer a presumptive identification. However, color tests are not available for all the analogues of fentanyl that may be encountered. In addition, color tests require that contact with the sample be made during its analysis. Therefore, always undertake these tests while donning the appropriate level of PPE.
Ion mobility spectrometry (IMS) is a useful method for the detection of fentanyl and its analogues because the limit of detection of these systems is quite low – in the nanogram-level range. This means that particles of fentanyl that are completely invisible to the naked eye, and even to light microscopes, can be detected and identified using this method. The ability to detect these trace quantities is the value of this method. Not only do IMS systems detect these substances at very low levels, but they also identify the analogue of fentanyl present. In addition, because the system uses microscopic amounts during the test, the responder is not exposed to high levels of the substance during the analysis. This is especially important when higher-potency fentanyl analogues like carfentanil are present. The primary point responders should consider when interpreting results from an ion mobility system is which fentanyl analogues are programmed to alarm in the system they are using. IMS systems, like other systems, will only alarm for drugs and analogues programmed into the system.
Infrared and Raman systems are go-to identifiers at scenes for the analysis of drugs, liquids, and other white powders. The primary advantage of both systems is that they can conclusively identify most drugs of abuse. In addition, they also can successfully identify fentanyl and its analogues when these analogues are present in the system’s library.
However, these systems are not trace detectors. The system must be a bulk substance (you must be able to see the powder or liquid sample). In addition, the concentration of the fentanyl compound in the sample must be relatively high (usually anywhere between 3 percent and 10 percent). Both infrared and Raman systems analyze only a small area of the sample. For this reason, if the sample is a mixture, carefully consider the meaning of a negative detection of fentanyl or its analogues when using these methods. For instance, if a 100-milligram street sample of heroin is laced with 2 milligrams of fentanyl, it’s possible that even if the sample is analyzed from a number of different locations, the fentanyl or its derivative may not be detected. From a personal safety perspective of the responder, Raman systems offer the advantage that they can analyze a sample without making direct contact with the sample. These systems routinely identify through translucent materials including clear glass and plastic baggies. They are, however, challenged by fluorescence, which makes it difficult for Raman systems to identify some drugs of abuse. Infrared systems, on the other hand, need to make contact with the sample, which is a potential exposure issue for the responder. However, infrared systems are immune to fluorescence, so drugs that fluoresce in the Raman are usually easy to identify using infrared.
It is important that all response agencies consider developing guidelines for safely responding to emergencies involving these dangerous drugs. This type of guidance, followed up with proper and sustained training, is critical. Regardless of the analogue of fentanyl encountered or the type of emergency scene to which responders are dispatched, they should understand the dangers present and take the appropriate actions to protect themselves and the public at large.
References
1. American Cancer Society. Opiod Pain Medicines for Cancer Pain. American Cancer Society. [Online] June 5, 2017. https://www.cancer.org/treatment/treatments-and-side-effects/physical-side-effects/pain/opioid-pain-medicines-for-cancer-pain.html.
2. Fowler, Ian. Medical Monday: Fentanyl “Lollipop” Supplants Morphine on Battlefield. Department of Defense Live. [Online] December 5, 2011. [Cited: June 5, 2017.] http://www.dodlive.mil/2011/12/05/fentanyl-lollipop-supplants-morphine-on-battlefield/.
3. American Pregnancy Association. Using Narcotics for Pain Relief During Childbirth. American Pregnancy Association. [Online] June 5, 2017. http://americanpregnancy.org/labor-and-birth/narcotics/.
4. Garimella, Veerabhadram and Cellini, Christina. “Postoperative Pain Control.” Clinics in Colon and Rectal Surgery. 3,2013;26:191-196.
5. United States Drug Enforcement Administration, Drug and Chemical Evaluation Section. Fentanyl Drug Chemical Information. United States Drug Enforcement Administration Diversion Control Division. [Online] December 2016. [Cited: June 4, 2017.] https://www.deadiversion.usdoj.gov/drug_chem_info/fentanyl.pdf.
6. Silsby HD, Druzich DJ and Hawkins MR. “Fentanyl Citrate Abuse Among Health Care Professionals.” Military Medicine. 4,1984;149: 227-228.
7. Douglas, Jeff. “Painkiller Patch Abuse Blamed for Deaths.” The Washington Post. June 16, 2006.
8. United States Drug Enforcement Administration. DEA Issues Carfentanil Warning to Police and Public. United States Drug Enforcement Administration. [Online] September 22, 2016. [Cited: June 21, 2017.] https://www.dea.gov/divisions/hq/2016/hq092216.shtml.
9. RehabCenter.Net. The Average Cost of Illegal Drugs on the Street. RehabCenter.net. [Online] [Cited: June 18, 2017.] http://www.rehabcenter.net/the-average-cost-of-illegal-drugs-on-the-street/.
1 0. Cicero, Theodore J. Ellis, Matthew S. Kasper, Zachary A. “Increase in self-reported fentanyl use among a population entering drug treatment: The need for systematic survelliance of illicitly manufactured opiods.” Drug and Alcohol Dependence, Aug 2017;177:101-103.
11. United States Department of Justice, Drug Enforcement Administration. Fentanyl: A Briefing Guide for First Responders. United States Drug Enforcement Administration. [Online] [Cited: June 6, 2017.] https://www.dea.gov/druginfo/Fentanyl_BriefingGuideforFirstResponders_June2017.pdf.
12. Frank, Richard G and Pollack, Harold A. “Addressing the Fentanyl Threat to Public Health.” The New England Journal of Medicine. February 16, 2017;605-607.
13. McDaniels, Andrea K. “Authorities Brace for More Overdoses after Maryland Deaths Linked to Elephant Sedative.” The Baltimore Sun. April 25, 2017.
14. Grant, Julie. Suspected Elephant Tranquilizer Carfentanil Seized in Drug Bust. Pittsburgh CBS Local News. May 4, 2017.
15 .Katz, Josh. “Drug Deaths in America Are Rising Faster Than Ever.” The New York Times. June 5, 2017.
16. United States Drug Enforcement Administration. Controlled Substances Schedules. United States Drug Enforcement Administration Diversion Control Division. [Online] [Cited: June 21, 2017.] https://www.deadiversion.usdoj.gov/schedules/.
17. – . Schedules of Controlled Substances: Temporary Placement of Acryl Fentanyl into Schedule I. Federal Register. 2017, Vol. 82, 105.
18. United States Drug Enforcement Administration, Diversion Control Division. NFLIS Brief: Fentanyl, 2001-2015. Springfield: United States Drug Enforcement Administrator, 2017.
19. Volkow, Nora D. America’s Addiction to Opiods: Heroin and Prescription Drug Abuse. Testimony to United States Congress, Senate Caucus on International Narcotics Control. May 14, 2014.
20. Sites, Brian D. Beach, Michael L. Davis, Matthew. “Increases in the Use of Prescription Opioid Analgesics and the Lack of Improvement in Disability Metrics Among Users.” Regional Anesthesia and Pain Medicine. 2014;(39)1:6-12.
21. Weaver, Jay and Ovalle, David. “Heroin Substitute Fentanyl, Not Infamous Flakka, Is Deadliest New Designer Drug.” Bradenton Herald. Sept 27, 2015.
22. The Economist. The Latest Scourge: Fentanyl is the next wave of America’s Opiod Crisis. The Economist. [Online] May 20, 2017. http://www.economist.com/news/leaders/21722189-criminalisation-not-right-way-approach-it-or-other-drugs-fentanyl-next-wave.
23. Tavernise, Sabrina. To Cut Abuse, F.D.A. Is Altering Painkiller Labor Rules. The New York Times. September 13, 2013.
24. Talbot, Margaret. The Addicts Next Door. The New Yorker. June 2017.
25. Cicero, Theodore J. Ellis, Matthew S. Surratt, Hilary L. “Effect of Abuse-Deterrent Formulation of OxyContin.” New England Journal of Medicine. July 12, 2012;367(2):188-189.
26. The National Institute for Occupational Safety and Health (NIOSH). Fentanyl: Preventing Occupational Exposure to Emergency Responders. Centers for Disease Control and Prevention. [Online] November 16, 2016. https://www.cdc.gov/niosh/topics/fentanyl/default.html.
27. Justice Institute of British Columbia. Handling of Suspected Drugs. Fentanyl Safety for First Responders. [Online] [Cited: June 26, 2017.] https://www.fentanylsafety.com/safe-handling/.
28. Position Statement of the American College of Medical Toxicology and American Academy of Clinical Toxicology. American College of Medical Toxicology. [Online] July 12, 2017. http://www.acmt.net/_Library/Fentanyl_Position/Fentanyl_PPE_Emergency_Responders_.pdf.
PAULINE E. LEARY, Ph.D., is a technical solutions engineer for Smiths Detection, Inc. She works with military, emergency-response, transportation, and critical-infrastructure customers in developing solutions to problems with detecting, identifying, and quantifying dangerous substances and other contraband in the field. Prior to joining Smiths in 2005, Leary worked as scientist performing physical testing within the R&D division of Purdue Pharma, LP. She has a bachelor of arts degree from Marist College, a master of science degree from John Jay College of Criminal Justice, and a Ph.D. from the Graduate Center of the City University of New York.
BRANDON A. GAYLE began his fire service career in 1997 with the Raleigh (VA) Fire Department and has served as a hazmat specialist for the department since 1999, currently as a lieutenant. He has been a certified fire service instructor for the North Carolina Office of the State Fire Marshal in the field of hazardous materials response since 2006. Gayle is the president of Gayle Training Solutions, LLC, which provides training and consulting services for companies such as Smiths Detection, Inc. and Federal Resources Supply Company. He has trained fire, EMS, law enforcement, hazmat responders, and military troops. He is a member of North Carolina Hazardous Materials Regional Response Team 4 and the North Carolina Urban Search and Rescue Task Force 8. H is a volunteer on the Wake County Local Emergency Planning Committee and is a member of the North Carolina Association of Hazardous Materials Responders.
DONALD G. GROSS began his career as a firefighter for the Durham (NC) Fire Department in 1998 and has held the rank of captain since 2009. He has also been serving as coordinator of hazmat operations since 2012. He is president of D&C Instruction, which has been providing hazmat training and consulting services domestically and internationally for the past 13 years. Gross has a BS in chemistry and a BA in biology from the University of North Carolina at Wilmington.
MICHAEL FRUNZI, Ph.D., is the senior product manager and subject matter expert for optical technology at Smiths Detection, Inc. He specializes in development, deployment, and global life-cycle management of handheld sensor products for CBRNe and narcotics identification applications for military, transportation, security, and emergency responder markets. He joined Smiths Detection six years ago; previously, he worked two years with Professor Nicholas Turro at Columbia University after receiving his Ph.D. in physical chemistry from Yale University in 2009.
Firefighter Training: Preplanning Your Preconnects
Improving Preconnect Function and Operation
Making Preconnects Work
Fire Engineering Archives

