By KAREN OWENS
Scenario: You and your driver have just finished restocking your vehicle and have marked in service from the last call when you are toned out for the next. You hear, “Medic 4, respond to Johnsonville Park for a 12-year-old male with a sports injury. Patient is on the sideline of the football field.” Knowing that it is football season, you prepare for a long list of potential injuries.
In 2001, athletes between the ages of five and 24 accounted for more than 2.6 million emergency department visits.1 With increased numbers of children involved in contact sports, it is no wonder that these incidents are increasing. Looking specifically at concussions, from the period of 1997 to 2007, the number of emergency department visits for 14- to 19-year-olds has more than tripled; between 30 and 58 percent of those visits were sports related. (1) With this increase in sports injuries-specifically concussions-it is important for emergency medical services (EMS) providers to have the knowledge, skills, and abilities to assess and treat concussions appropriately.
A concussion is classified as a mild traumatic brain injury (TBI).2 It occurs when an individual suffers a direct blow to the head or face. The mechanism of injury results in acceleration/deceleration and/or rotational forces on the brain, causing injury to multiple areas of the brain.3 These injuries can cause bleeding and bruising in the brain tissue, leading to multiple signs and symptoms of concern as well as permanent impairment. Because of the mechanics of most sports, the potential for concussion injuries is significant.
On arrival at the football field, you are escorted to the sidelines and introduced to your patient, a 12-year-old male football player who is sitting on a bench. His helmet has been removed, but he is still wearing his shoulder and chest pads. As you begin talking to him, you notice that he appears lethargic, and he complains of a headache.
Assessment
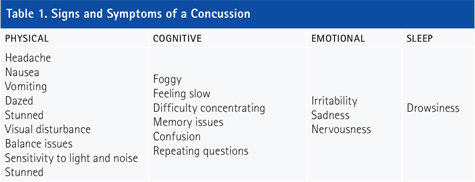
As an EMS provider, it is important to not only recognize the signs and symptoms of concussions but also to associate them with a potential diagnosis of concussion to ensure appropriate field treatment is initiated. When assessing a patient that you believe has a concussion, remember that fewer than 10 percent of athletes who sustain a concussion lose consciousness. (3) The signs and symptoms of concussion are often subtle and can mimic other medical conditions such as dehydration or stomach upset. Table 1 lists the signs and symptoms of a concussion and categorizes them based on the physical, cognitive, emotional, and sleep impacts. If EMS is called immediately following the injury, there is a chance that the patient may complain of only a few symptoms, making it harder to determine if you are dealing with a concussion. For this reason, it is important to conduct a thorough physical assessment and patient interview.
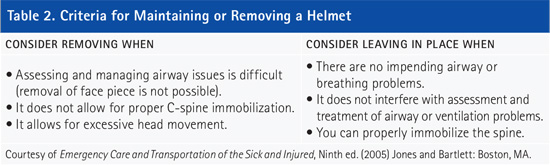
As with any call, focus your assessment on the immediate life threats. Once scene safety and appropriate personal protective equipment are in place, rule out the need for C-spine stabilization. In many sports-related injuries, precautionary C-spine stabilization may be recommended, but state and local protocols are rapidly evolving in this area. Follow your local protocols. Additionally, when a helmet or headgear is worn in sports such as football, baseball, hockey, wrestling, or lacrosse, consider maintaining or removing the helmet. Table 2 provides general criteria to help determine whether to maintain or remove a helmet.4
Although airway, breathing, and circulation assessment are high priorities, the interview and assessment of the patient’s mental status will provide significant information on his status and the impact of the injury. Assess any patient suspected of having a concussion for retrograde (before the injury) and antegrade (after the injury) memory loss.5 The acronym SAMPLE can provide information on actions and activities prior to the incident such as last oral intake and events leading up to the incident. Interviewing coaching staff can help provide information on behavior and symptoms displayed after the injury as well as provide corroboration with information you obtain from the patient or bystanders.
Your interview with the patient reveals that he experienced a helmet-to-helmet hit while running a play. He experienced no loss of consciousness, but he admits he does not remember the pre-play huddle or walking to the sidelines. He complains of a slight headache (4 on a scale of 1 to 10) and some nausea but no difficulty breathing. You package him for transport and move him to the ambulance.
Treatment
Diagnosing a concussion is based on a constellation of signs and symptoms, not just on loss of consciousness. As previously mentioned, it is quite possible to sustain a significant concussion with no loss of consciousness whatsoever. The ability of a field provider to conduct a thorough exam is limited, and the inability to make a diagnosis is fraught with potential for permanent disability should an athlete return to play and be reinjured. Any athlete with a suspected concussion must be removed from play and medically assessed either at an emergency department or by his personal physician. No athlete should be allowed to return to play following a head injury even if his signs and symptoms appear completely resolved.
EMS care for a patient with a potential concussion should remain focused on treating signs and symptoms. Treatments might include spinal motion restriction, airway management (as necessary) to include supplemental oxygen, and respiratory support. Consider transporting the patient with dimmed or no lights or sirens (unless the patient is emergent) to minimize the amount of stimulation that the patient has to process.
Remember, this may not be the first brain injury the athlete has suffered. Many players will experience concussion-like symptoms without fully recovering before returning to play, despite recommendations against this. As a result, you may see secondary injury, causing more significant damage to the brain with a greater chance of this patient deteriorating as the call progresses.
The seriousness of concussions in children who play contact sports is receiving greater attention. As a result, there is increased training in recognizing the signs and symptoms of concussions and the steps to take to minimize the impact of the injury. As an EMS provider, you must ensure that you not only recognize the potential for injury but also remove the athlete from play, provide appropriate supportive care, and transport or refer to a physician for complete assessment. Ultimately, the long-term health and wellness of an injured player could depend on your actions.
REFERENCES
1. Merkel DL and JT Molony Jr. (April 2012). “Medical sports injuries in the youth athlete: Emergency management.” International Journal of Sports Physical Therapy, Vol. 7, Number 2.
2. Edenburn D (February 1, 2012). “Concussion management.” Accessed June 4, 2015 from www.emsworld.com/article/10611569/concussion-management.
3. Halstead ME, Walter KD, and the Council on Sports Medicine and Fitness (2010). “Sport-related concussion in children and adolescents,” Pediatrics. Accessed May 15, 2015, from pediatrics.aapulibcations.org.
4. American Academy of Orthopaedic Surgeons, The (2005). Emergency Care and Transportation of the Sick and Injured, Ninth ed., Jones and Bartlett: Boston, MA.
5. McEvoy M. (2012, Jan 1.) “Heads up on teen athlete concussions.” Accessed June 10, 2015 from http://www.boundtreeuniversity.com/columnists/mike-mcevoy/articles/1211532-Heads-up-on-teen-athlete-concussions.
KAREN OWENS is the emergency operations manager for the Virginia Office of EMS, where she has been employed since 2001. Her duties include oversight of the emergency operations training programs including mass casualty incident management, terrorism awareness, and vehicle rescue. Owens has a BA degree in psychology and an MA degree in public safety leadership. She is a Virginia-certified firefighter and has been a Virginia EMT-B instructor since 2002. Owens is the author of Incident Command for EMS, published by Fire Engineering.

