By MICHAEL M. DUGAN and TERRENCE BURNS
Not long ago, hospitals posted “Use of Flammable Anesthetics Prohibited” signs throughout critical care units, emergency rooms, and operating rooms. During that era, anesthetic vapors were volatile and flammable. Patient side effects such as nausea and vomiting were profound. This led to the development of modern anesthetic ethers that were not fire or explosion hazards. For the anesthesiologist, onset and offset of drug effects were more predictable, and the side effect profile was much better. For the hospital administrator, patient satisfaction and operating room turnover improved.
Flash forward to 2014. Anesthesiology has evolved as a science and a profession. New drugs and anesthesia techniques provide patients with more options than ever before. The use of general anesthesia has decreased, while regional anesthesia has increased. Many operations can be done with conscious patients who are sedated. However, sedated patients often require open delivery of oxygen through cannula or a mask.
 |
 |
| (1, 2) Dedicated gas shut-off valves outside the operating room entrance. (Photos by Terrence Burns.) |
Bacteria are smarter than you think! Bacteria are survivors, changing their game plan to meet any challenge the medical profession throws at them. Wound infections are caused by surgical morbidity, mortality, and economic cost. If a hospital has too many surgical wound infections, it can be penalized financially; hence, the development of surgical skin prep solutions with isopropyl alcohol, which is very effective against bacteria but is also flammable.
Operating rooms use a great deal of electricity. The electrosurgical unit (ESU) delivers electrical energy at the tip of a pencil point. The ESU allows the surgeon to cut or cauterize open tissue, thereby decreasing blood loss and operative time. As tissue boils, tiny sparks can be generated on the surface of the skin in a controlled fashion.
This sounds familiar to every firefighter-the fire triangle at work in the unique setting of a hospital operating room. Under certain circumstances, oxygen (open), fuel (alcohol), and heat (ESU) can combine to set a patient on fire. Patients’ injuries range in severity from minor to patient death.
 |
| (3) Ordinary materials you will find in an operating room. |
In 2008, the American Society of Anesthesiologists published Practice Advisory for Prevention and Management of Operating Room Fires. A disturbing trend was recognized: A problem from yesteryear was making a comeback. The scientific community of anesthesiologists developed a task force to study the problem, and guidelines were set forth for practice. The technical information and the science behind the guidelines are well grounded. The next challenge was to educate all members of the operating room team in how to prevent and manage a fire in the operating room.
THE OPERATING ROOM TEAM
Anesthesiologists, surgeons, nurses, and surgical technicians have personality traits similar to firefighters; they are familiar with stressful situations and can operate a wide range of technical equipment. Time constraints occur on a routine basis; drills and training sessions are part of their continuing education, and they function as part of a team.
In the operating room, they are the fire department (at least for the first five to 10 minutes of a fire). Prompt, immediate intervention is crucial to improving outcome and minimizing patient injury. An effective example, by way of comparison, is an aircraft carrier in the middle of the ocean. Every person on board the ship has been trained to fight fires. Why? Because they cannot wait for fire trucks to pull up and save the day.
OXYGEN
Nearly 100 percent of operating room patients require supplemental oxygen. Ensuring that the human body receives-at all times-more oxygen than it can consume is a mainstay of anesthetic practice. Oxygen can be delivered to the patient as an inhaled gas that cells can use to carry out aerobic metabolism. Another source of oxygen is nitrous oxide, which is blended with oxygen and delivered to the patient as an anesthetic gas. Both oxygen and nitrous oxide support combustion, lower the ignition temperature of ordinary materials, and enhance the intensity of any fire.
Consider some real-life examples: The Apollo 1 disaster in 1963 killed three astronauts in a flash fire at a training session. The crew was working on the ground in an oxygen-enhanced atmosphere. A spark touched off a fire, and the astronauts were dead in 30 seconds. Also consider professional race car drivers, who attain high speeds in nitrous oxide-powered vehicles.
In the operating room, patients are either conscious or asleep under general anesthesia. By definition, general anesthesia means a patient cannot protect his or her airway. Therefore, they usually are intubated with a cuffed endotracheal tube. The breathing circuit is sealed, and there is no leakage of oxygen to the surrounding atmosphere.
Alternatively, conscious patients usually receive open oxygen delivery by mask or nasal cannula. This creates an oxygen-enriched atmosphere around the patient. Molecular oxygen has a density greater than room air; it will displace room air and persist, unseen, around the patient’s body. It will fill any dead space under surgical drapes and can leak into the surgical field.
 |
| (4) An old problem makes a return to the operating room. Because of fires caused by or contributed to by oxygen and flammable anesthetics, the use of flammable anesthetics was restricted in the past. |
FIRE DEPARTMENT ROLES
The local fire department has to do some legwork to help eliminate potential fires and reduce risks. It must be aware of and identify all local areas that perform surgery, from local hospitals to a medical office that performs surgical procedures such as colonoscopies, endoscopies, and so on. All of these places are oxygen-enriched areas; you will need to know what to expect on arrival for a report of a fire at these facilities.
The first thing you must look for during an operating room fire containing an unconscious patient under general anesthesia who is opened for a procedure is the staff that is in place for an emergency. If the hospital has an operating room with a fire extinguisher, the local professional must determine if it is the proper type of extinguisher. If the surgery requires opening the patient or if the patient is unconscious, using a dry chemical extinguisher is dangerous; those small contents particles can enter into an open wound or airway. Therefore, those spaces will require a carbon dioxide (CO2) extinguisher. If the local professional was never informed of the need for a CO2 extinguisher, do you expect to find one?
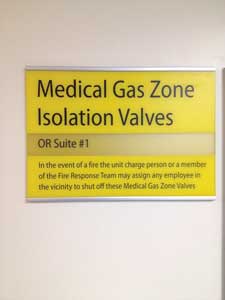 |
| (5) The pull-away cover for gas shut-off valves must be removed to access the valves. |
The second consideration is the amount of contaminates you will bring into a sterile area, which will most likely lead to an infection in the patient and, depending on the patient’s medical condition, could be deadly.
A fire department must be proactive and set up education drills for hospital staff and medical facilities so they know what to do in an emergency. It is also recommended that the fire department train hospital staff on what the staff needs to do with a patient during an emergency. The consequences of responding to these dangerous situations must be addressed before an incident occurs to protect the life of the patient. The best way to begin this process is to identify any place of surgery and open the lines of communication between the medical community and the fire department.
MICHAEL M. DUGAN is a 36-year fire service veteran and a 27-year member of the Fire Department of New York (FDNY), where he retired as captain of Ladder Company 123 in Crown Heights, Brooklyn. As a lieutenant, he served in Ladder Company 42 in the South Bronx. While assigned as a firefighter in Ladder Company 43, in Spanish Harlem, he received the James Gordon Bennett Medal in 1992 and the Harry M. Archer Medal in 1993, FDNY’s highest award for bravery. He was a volunteer firefighter in Halesite, New York. He lectures on truck company operations, building construction, size-up, and today’s fire service.
TERRENCE BURNS, MD, is a board-certified anesthesiologist practicing in Buffalo, New York. He is an assistant clinical professor of anesthesiology at SUNY-Buffalo. Prior to medical school, Burns worked for five years as a firefighter at the Buffalo (NY) Fire Department’s Engine 3. He is a guest lecturer on operating room fires for the New York State Society of Anesthesiologists.
Fire Engineering Archives

