BY DENISE L. SMITH, JEANNIE HALLER, WESLEY K. LEFFERTS, ERIC M. HULTQUIST, AND PATRICIA C. FEHLING
Firefighters perform strenuous work in dangerous and unpredictable environments. Despite the numerous dangers on the fireground, the leading cause of line-of-duty deaths (LODDs) among firefighters in the United States is sudden cardiac death, which accounts for approximately 50 percent of deaths.1 Several research studies have shown that firefighting may serve as a trigger for a sudden cardiac event in susceptible individuals; however, the precise mechanisms by which firefighting may lead to a sudden cardiac event are not well defined.2 Figure 1 presents a theoretical model that depicts the relationship between firefighting and cardiovascular strain and the relevance to the fire service.
Firefighting involves strenuous work and is performed while wearing personal protective equipment (PPE). Heat stress frequently occurs on the fireground because of the combination of muscular work, impaired heat dissipation associated with the wearing of PPE, and radiant heat. Heat stress results in profuse sweating, which often leads to dehydration. Muscular work, heat stress, and dehydration all contribute to cardiovascular strain (high heart rate, high cardiac output, enhanced blood clotting potential). Cardiovascular strain is a major concern for all firefighters because it can lead to the early onset of fatigue, which may impair performance or force firefighters to stop working. Additionally, high cardiovascular strain is a major safety concern in firefighters with an underlying disease because it may lead to a cascade of events (e.g., plaque rupture, clot formation, ischemia) that result in a sudden cardiac event.
 |
| Figure 1. Firefighting and Cardiovascular Strain |
Although numerous field studies have shown that firefighting leads to increased cardiovascular strain, these studies were not designed to isolate the independent effects of heat stress and dehydration on the cardiovascular system. A better understanding of the independent contributions of these two challenges may allow the fire service to develop targeted countermeasures to prevent and reduce injuries and deaths associated with cardiac strain.
Therefore, we conducted a laboratory study that allowed us to investigate the independent effects of heat stress and dehydration on cardiovascular strain. Although the laboratory study did not include the physical and psychological strain encountered during actual firefighting emergencies, it allowed us to tightly control the level of work and standardize conditions. Importantly, we used an exercise/work protocol and conditions that were relevant to firefighting in terms of the intermittent nature of the work and the levels of heat stress and dehydration induced.
Study Design
This study was completed as part of a larger, comprehensive study to investigate the effects of heat stress and dehydration on cardiovascular function. A full description of the study design and the results can be found in peer-reviewed publications.3,4,5
Briefly, 12 healthy, physically active, college-age men completed three different experimental trials on separate days. Since heart rate is influenced by several factors, we standardized testing procedures by performing trials at the same time of day and imposing caffeine, alcohol, and strenuous exercise restrictions to keep these factors consistent for all trials. Additionally, all participants ate a standardized meal prior to each day of testing.
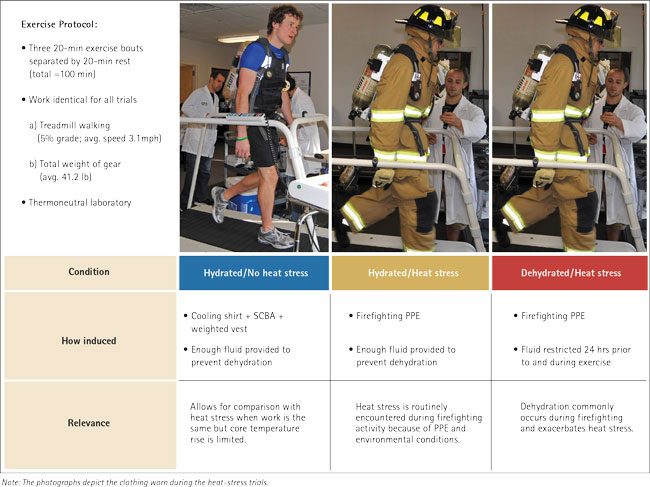 |
| Figure 2. Experimental Design and Conditions |
During each trial, the participant performed a 100-minute intermittent exercise (work) protocol; however, the degrees of heat stress and dehydration were manipulated by varying the clothing worn and the fluid intake to create three different experimental conditions: hydrated/no heat stress, hydrated/heat stress, and dehydrated/heat stress (Figure 2). We were interested in assessing the influence of heat stress (induced by walking in PPE) and the effect of a combination of heat stress and dehydration on thermal and cardiac strain. Thus, we included a condition in which participants did the same work (walking at the same speed and grade wearing the same weight), but in one condition we limited the increase in core temperature by having participants wear a cooling vest. The following section details how we manipulated these variables.
Manipulated Variables Heat Stress
To mimic moderate heat stress (core temperature < 101.3°F) that has been reported during firefighter drills,6,7 participants walked on a treadmill while wearing full structural firefighting PPE. Firefighting PPE was identical for all participants and consisted of turnout pants and coat, boots, gloves, hood, helmet, and self-contained breathing apparatus (SCBA) (average weight of gear: 41.2 pounds).
No Heat Stress
To minimize heat stress, participants walked on a treadmill while wearing a cooling shirt that circulated cool water next to the body through embedded tubing. Participants also wore a weighted vest and carried an SCBA. Thus, the total weight carried matched the weight of the heat-stress trials in which PPE (41.2 pounds) was worn. This ensured that the amount of work done in all trials was the same.
Hydrated
In the hydrated trials, participants started the trial fully hydrated, and the fluid lost through sweating during the protocol was replaced by fluid ingestion during recovery periods. To ensure proper hydration at the start of the exercise trial, participants were given between 34 and 50 ounces (between two and three liters) of water to drink in the 24 hours prior to testing, and urine specific gravity was tested to ensure participants were not dehydrated. Water and sports drinks were provided during testing to match fluid loss (as estimated during familiarization trials) and minimize the change in body weight.
Dehydrated
In the dehydrated trial, participants started the trial in a mildly dehydrated state (a one- to two-percent body weight loss), and additional dehydration was induced by restricting fluid during testing. Mild dehydration at the start of testing was employed because several research studies have shown that firefighters report to work or training in a dehydrated state.8,9,10 Mild dehydration was achieved by providing participants with only between 17 and 25 ounces (between one and 1.5 liters) of water to drink during the 24 hours preceding testing. Minimal fluid [~1 cup (240 mL)] was provided during the testing protocol. The goal was to induce three-percent body weight loss between the end of the protocol and the previous 24-hour measurement of body weight.
Exercise Protocol
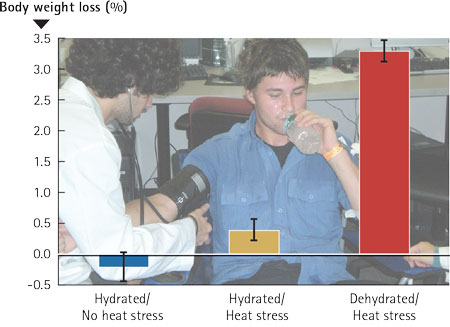 |
| Figure 3. Body Weight Loss |
The 100-minute protocol consisted of three 20-minute bouts of treadmill walking at a moderate intensity with a 20-minute rest between bouts to mimic the work/rehab cycles encountered during prolonged firefighting or training drills. For each participant, the work performed during each trial was kept constant. The grade was set at five percent, and the speed averaged 3.1 miles per hour.
Measurements
We assessed hydration status at the start of the experimental trial by measuring urine specific gravity. Body weight was measured 24 hours prior to the experimental trial, before the exercise protocol, and immediately after the exercise protocol. Heart rate was measured continuously throughout the 100-minute intermittent exercise protocol using a heart rate monitor. Core temperature was measured throughout the protocol using an ingestible pill.
Results and Discussion
Figure 3 shows total body weight loss between the 24-hour pretrial measurement and the postexercise measurement. Results indicate that the criteria for the hydrated and dehydrated conditions were met-body weight change was minimized (within 0.4 percent) for both hydrated trials, and body weight loss was approximately three percent for the dehydrated trial.
Core temperature rose during exercise and into the first two minutes of recovery and then decreased during recovery during all trials (Figure 4). By design, the core temperature was higher during the heat-stress condition than the no-heat-stress condition. Differences in core temperature among the trials were visible by the end of the first exercise bout and became more pronounced as the protocol continued. In the hydrated/no heat stress trial, core temperature increased by 1.1°F between the start and completion of the protocol. In comparison, core temperature increases were between two and 2.5 times higher in the heat-stress trials; the core temperature increased by 2.2°F during the hydrated/heat stress trial and by 2.7°F in the dehydrated/heat stress trial. The ~0.5°F difference between the hydrated/heat stress and dehydrated/heat stress trials clearly indicates that dehydration exacerbates thermal strain.
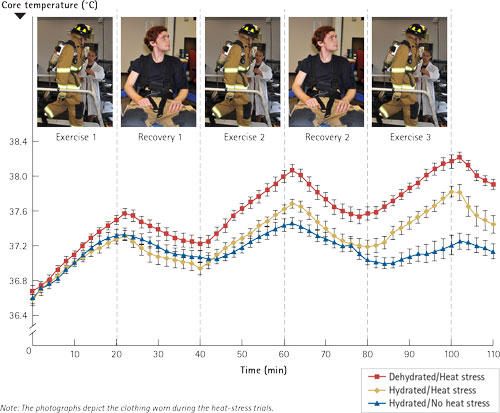 |
| Figure 4. Core Temperature During Intermittent Exercise |
The increase in core temperature that we found in the dehydrated/heat stress trial is similar to increases that have been reported with live fire training drills.(6),11 It is also important to note that the recovery periods allowed core temperature to decrease toward baseline values. However, even after 20 minutes of recovery, the core temperature was not back to baseline, and each successive bout of exercise resulted in a higher core temperature.
As expected, heart rate increased during exercise and decreased during recovery in all three conditions. Figure 5 shows the pronounced differences in heart rate (HR) between the heat stress trials and no-heat-stress trial throughout the protocol. Firefighters know that PPE adds to the work they do, but these results clearly demonstrate the magnitude of the physiological burden associated with PPE. In the hydrated trials, HR reached 105 beats per minute (bpm) in the no-heat-stress condition and 152 bpm in the heat-stress condition at the end of Exercise 3-a difference of nearly 50 bpm. Importantly, the participants carried the same amount of weight. Therefore, the 50 bpm higher HR in the two heat-stress trials (caused by wearing PPE) cannot be attributed to weight. Rather, this difference reflects the strain induced by the effect of PPE on core temperature and perhaps to some degree the increased effort of walking in bulky clothing. Furthermore, the increase in heart rate when dehydration was superimposed on heat stress is clearly evident in Figure 5. When dehydration was coupled with heat stress, the heart rate was six bpm greater compared with heat stress alone.
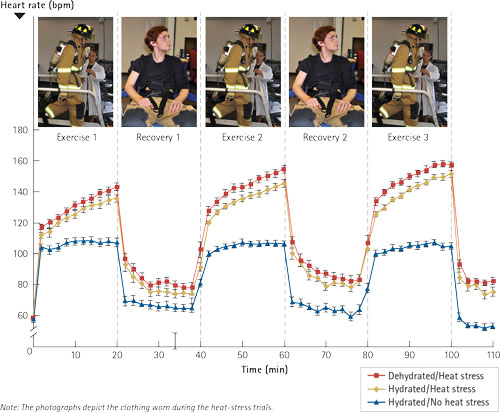 |
| Figure 5. Heart Rate During Intermittent Exercise |
This study confirms what firefighters know well from experience-PPE imposes substantial cardiac strain during work. However, the magnitude of the physiological strain of PPE is likely far greater than is generally known and is not entirely attributed to the weight of the gear. Additionally, our results indicate that dehydration further exacerbates cardiac strain during work, which is likely less apparent to many firefighters.
Relevance for Firefighters
Firefighters routinely face the twin challenges of heat stress and dehydration on the fireground, and the effects of these factors on cardiac strain are often intertwined. This study showed that moderate heat stress induced by walking in PPE, consistent with that documented during live-fire training exercises, caused substantial cardiac strain (HR = 150-160 bpm). Our study also showed that moderate dehydration (three percent) exacerbated thermal strain and further contributed to cardiac strain experienced with heat stress.
On the fireground, heat stress is an unavoidable challenge that results from working in heavy, encapsulating PPE that limits heat dissipation and from environmental conditions. Dehydration is a potential consequence of firefighting and of inadequate fluid intake in general, but to a large extent dehydration is avoidable. Importantly, firefighters can take a proactive approach to combat the adverse effects of heat stress and dehydration.
Recommendations
To mitigate the detrimental consequences (early fatigue, impaired job performance, or sudden cardiac event in susceptible individuals) of cardiac strain resulting from heat stress and dehydration during strenuous firefighting activities, firefighters should do the following:
- Receive an annual medical evaluation consistent with National Fire Protection Association (NFPA) 1582, Standard on Comprehensive Occupational Medical Program for Fire Departments,12 and performed by a physician familiar with the physiological demands of firefighting. In addition to clearing a firefighter for duty, findings of this exam should be used to aggressively manage risk factors for cardiovascular disease.
- Engage in regular physical exercise to improve work performance, enhance cardiovascular function, improve thermoregulation, and provide cardioprotection.
- Ensure proper hydration before emergency operations and consume fluids during/following operations to rehydrate. Hydration status can be monitored using a simple urine chart.
- Adopt NFPA 1584, Standard on the Rehabilitation Process for Members During Emergency Operations and Training Exercises,13 and ensure that incident rehabilitation is established for emergency operation and training drills. Rehabilitation provides an opportunity for rest, rehydration, and active cooling. Additionally, during rehabilitation, EMS should monitor vital signs and observe firefighters for signs suggestive of the need for further medical care.
Authors’ note: This study was supported by a FEMA-AFG grant to D. Smith, PI (EMW-2010-FP-01992). A complete report of this study is available from our Web site: http://www.skidmore.edu/responder/.
References
- Fahy, RF, PR LeBlanc, and JL Molis. (2014) Firefighter Fatalities in the United States-2013. Quincy, MA: National Fire Protection Association, 2014. http://www.nfpa.org/newsandpublications/nfpa-journal/2014/july-august-2014/features/firefighter-fatalities.
- Smith, DL, DA Barr, and SN Kales. (2013) “Extreme sacrifice: sudden cardiac death in the US fire service.” Extreme Physiology & Medicine, 2013; 2:6. http://www.extremephysiolmed.com/content/2/1/6.
- Fehling, PC, JM Haller, WK Lefferts, EM Hultquist, M Wharton, TW Rowland, and DL Smith. (2015) “Effect of exercise, heat stress and dehydration on myocardial function.” Occupational Medicine, 2015; 65(4):317-323. http://www.ncbi.nlm.nih.gov/pubmed/25868467/
- Lefferts, WK, KS Heffernan, EM Hultquist, PC Fehling, and DL Smith. (2015) “Vascular and central hemodynamic changes following exercise-induced heat stress.” Vascular Medicine, 2015; 20(3):222-229. http://www.ncbi.nlm.nih.gov/pubmed/25939655.
- Smith, DL, JP DeBlois, M Wharton, PC Fehling, and SM Ranadive. (2015) “Effect of moderate exercise-induced heat stress on carotid wave intensity.” European Journal of Applied Physiology. 2015; 115(10):2223-30. http://www.ncbi.nlm.nih.gov/pubmed/26112919.
- Smith, DL, SJ Petruzzello, MA Chludzinski, JJ Reed, and JA Woods. (2005) “Selected hormonal and immunological responses to strenuous live-fire firefighting drills.” Ergonomics, 2005; 48(1):55-65. http://www.ncbi.nlm.nih.gov/pubmed/15764306.
- Colburn, D, J Suyama, SE Reis, J Morley, FL Goss, Y-F Chen, CG Moore, and DA Hostler. (2011) “Comparison of cooling techniques in firefighters after a live burn evolution.” Prehospital Emergency Care, 2011; 15(2):226-232. http://www.ncbi.nlm.nih.gov/pubmed/21294631.
- Brown, J, A. Derchak, A Bennett, M Lepore, and S Edwards. (2007) “Impact of pre-participation hydration status on structural firefighter cardio-respiratory response to standard training activities.” Medicine & Science in Sports & Exercise, 2007; 39(5):S153. http://www.researchgate.net/publication/246623010_Impact_of_Pre-Participation_Hydration_Status_on_Structural_Firefighter_CardioRespiratory_Response_to_Standard_Training_Activities_1195.
- Espinoza, CA and M Contreras. (2007). Safety and performance implications of hydration, core body temperature and post rehabilitation Orange County Fire Authority, Wellness and Fitness Program. Irvine, CA. http://www.mcftoa.org/wp-content/uploads/2008/12/hydrationstudy.pdf.
- Horn, GP, J Deblois, I Shalmyeva, and DL Smith. (2012) “Quantifying dehydration in the fire service using field methods and novel devices.” Prehospital Emergency Care, 2012; 16(3): 347-355. http://www.tandfonline.com/doi/abs/10.3109/10903127.2012.664243?journalCode=ipec20“>http://www.tandfonline.com/doi/abs/10.3109/ 10903127.2012.664243?journalCode=ipec20.
- Fernhall, B, CA Fahs, G Horn, T Rowland, and D Smith. (2012) “Acute effects of firefighting on cardiac performance.” European Journal of Applied Physiology, 2012; 112(2):735-741. http://www.ncbi.nlm.nih.gov/pubmed/21660460.
- National Fire Protection Association. NFPA 1582, Standard on Comprehensive Occupational Medical Program for Fire Departments. Quincy, MA: National Fire Protection Association, 2013. http://www.nfpa.org/.
- National Fire Protection Association. NFPA 1584, Standard on the Rehabilitation Process for Members During Emergency Operations and Training Exercises. Quincy, MA: National Fire Protection Association, 2015. http://www.nfpa.org/.
DENISE L. SMITH, PH.D., is the director of the First Responder Health and Safety Laboratory and professor of Health and Exercise, Skidmore College, Saratoga Springs, New York.
JEANNIE HALLER, MS, is a research associate with the First Responder Health and Safety Laboratory.
WESLEY K. LEFFERTS, MS, is a research associate with the First Responder Health and Safety Laboratory.
ERIC M. HULTQUIST, BS, is a research associate with the First Responder Health and Safety Laboratory.
PATRICIA C. FEHLING, PH.D, is chair and professor of the Health and Exercise Sciences, Skidmore College, Saratoga Springs, New York.
IFSI Study Underway on Firefighter Health
The Role of Heat Stress and PPE
Cardiovascular Training for Firefighters
More Fire Engineering Issue Articles
Fire Engineering Archives

