By Daniel DeGryse
Do you know what an “opioid” or an “opiate” is? Possibly, if I use the words “codeine,” “morphine,” “hydrocodone,” “methadone,” “oxycodone,” or “fentanyl,” you most likely would know I am talking about pain relievers. I would like to offer you a general understanding of the two and how they affect us. Opiates are alkaloids, natural substances that are derived from opium poppy. Alkaloids include morphine; codeine; opium; and, depending on the source of information, heroin. Heroin is an illicit drug manufactured with morphine, making it “semisynthetic.” Opioids, whether synthetic or semisynthetic, are drugs that are manufactured to mimic the effects of opiates. Even though opioids are synthetic, they can have more effects on our bodies than opiates. Further, although all opiates are opioids, not all opioids are opiates. Presently, because opiates and opioids attach to the same opioid receptors in our bodies, it has become common to refer to both as “opioids.”
Opioid Epidemic
To offer a perspective on the significance of the opioid crises across America, following are statistics from the 2017 census data as they relate to the nearly 327 million Americans in the United States. Following are some data collected by the American Society of Addiction Medicine in 2015:
• Two million people, ages 12 and older, had a substance use disorder involving prescription pain relievers, and 591,000 had substance use disorders involving heroin.
• Drug overdose is the leading cause of accidental deaths in the United States.
• In 2015, the United States experienced 52,401 lethal drug overdoses. Of those, 20,101 were related to prescription pain relievers and 12,990 were related to heroin.
To complicate the opioid crisis even more, in a 2014 survey of people in treatment for opioid addiction, 94 percent of the respondents self-reported they chose heroin because prescription opioids were too expensive and harder to obtain.

(1) The Florian room. (Photos courtesy of the Rosecrance Florian Program.) (
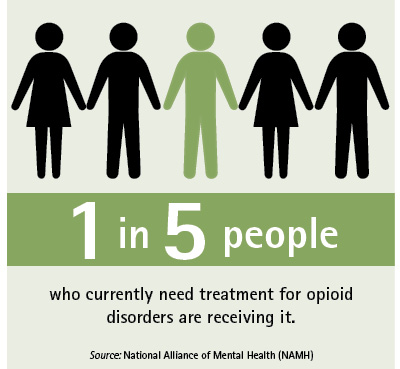
Further, the National Alliance on Mental Health reported that only one in five people who currently need treatment for opioid use disorders are receiving it. Opioid misuse, abuse, and addiction are gaining national attention. We frequently see news stories regarding individuals of all classes, backgrounds, education levels, ages, and so on who are struggling with their addiction and have loved ones struggling with addiction or who have lost their lives to these drugs.
According to Illinois Lieutenant Governor Evelyn Sanguinetti, “A lot of times, we think we know what these folks look like, but we don’t. This issue knows no neighborhood, no color, and no class.”
Raymond Garcia, medical director of the Harrison Campus for adults at Rosecrance Health Network, echoed Sanguinetti’s sentiment: “The chair in my office knows everybody,” said Garcia. “It sees homeless people and heads of companies.”

(2) The Rosecrance Florian helmet.
In the 2013 and 2014 National Survey on Drug Use and Health, 50.5 percent of people who misused prescription painkillers obtained them from a friend or relative for free; only 22.1 percent were prescribed by a doctor. Furthermore, as people use opioids regularly, their tolerance increases, warranting more pills for the same effect, and they may not be able to maintain their source for them. This can lead them to turning to alternative ways for obtaining these medications and even switching from prescription drugs to cheaper illicit ones like heroin.
Opioids and Fire Personnel
Now, consider one specific population, members of the fire service. Members of the fire service experienced 68,085 injuries in 2015, according to the National Fire Protection Association. They appear to be at a greater risk than the general population for job-related injuries. Physically, before they even begin work at a scene, they don protective gear and carry equipment that can range in weight from 45 to 77 pounds. They then face unpredictable scenes that include vehicle accidents, gas investigations, fire involving intense heat and dangerous structures, exposure to gases and chemicals considered hazardous materials, and other hazards. Aside from the physical challenges they face, they attend to a multitude of civilians of all ages who may be injured, burned, abused, dead, or decomposing. In addition, they must address and deal with the secondary victims on the scene that include family members, friends, and bystanders.
When in Pain, Ask Questions
Should you experience an injury or have a physical condition or ailment that warrants a prescription for pain medication, please become informed. Discuss with your doctor your condition and the plan for recovery. Is there a treatment? If so, and it involves pain management, what will be the time frame for the medication, and are there medications other than opioids that can see you through treatment? If opioids are warranted, discuss your options for types of medication. If you have a chronic condition and are prescribed opioids, discuss which one you will be using, its effects on your whole body, potential side effects, and how to properly and effectively use it.
In 2015, according to the U.S Department of Health and Human Services, 15,281 deaths were attributed to overdosing on commonly prescribed opioids, and 12,989 deaths were attributed to overdosing on heroin. As a precaution, inquire about prescription naloxone, a medication that blocks the opioid receptors and can counteract an overdose. Opioid overdose leads to respiratory depression; naloxone counters this effect and could be lifesaving in the event of an overdose. Include your significant other, other family others, or close friends in on what medication you are taking and why.
As a first responder, you know you are in a safety-sensitive position and that, therefore, your department most likely will place you on sick leave while you are taking prescription opioids. To further provide support for yourself, ask others to check on you while you are away from work so you can stay connected. Make them aware of the side effects and signs of medication overuse so they can help you stay on track in using the medication safely and effectively.
In November 2016, the Federal Drug Administration (FDA) published a checklist of questions for individuals to ask their doctors prior to taking a prescription opioid. It is available at https://www.fda.gov/ForConsumers/ConsumerUpdates/ucm529517.htm. If you are using a prescription opioid, how long have you been using it? Has your dosage increased? If you do not take the medication, do you experience any physical symptoms? Do you alter the medication by crushing it or dissolving it to snort or inject to get a more intense effect? Do you take it for reasons other than physical pain? Have you mixed or combined other substances while taking the medication? Many view prescription pain medications as “safe”; they do not consider the possibility of dependence; however, an early sign of potential problems is withdrawal symptoms. Some of these symptoms can occur within hours after not taking medication and are synonymous with symptoms of common ailments. It is important to be vigilant in your well-being so you do not mistake withdrawal for an illness or a side effect. Nausea or vomiting, runny nose, diarrhea, chills, muscle aches, and anxiety are some symptoms of withdrawal.
Misuse falls into three categories: taking prescribed pain medication in a manner other than that prescribed, taking someone else’s pain medication, or taking pain medications to feel euphoric (high). Once on one of these paths, a person can slip into dependence and, ultimately, an addiction to the medication.
The Effects
Opioid receptors are located throughout our body. Opioid drugs attach to the receptors, which in turn send out erroneous messages throughout our bodies regarding the level of pain we are experiencing. Hence, it is not actually reducing the pain but our perception of it. Another effect of opioids is that they produce a feeling of euphoria or “high.” Once attached to the opioid receptors, they block GABA—an amino acid that acts as an inhibitory neurotransmitter in our central nervous system and controls the release of dopamine from functioning properly. Dopamine is a naturally occurring neurotransmitter released during pleasurable activities. Therefore, with GABA unable to prevent dopamine from being released, opioids create a constant release of dopamine, and when the euphoric effect wears off, it can create a swing in emotion to a somewhat depressed state. This factor can allow dependency on the drugs to begin to take root. In addition, extended use and increased tolerance can lead to taking increased quantities, which can potentially cause permanent damage to the brain and its overall functioning.
Alternatives to Opioids
I’ve suffered multiple injuries throughout my years in the fire service, resulting in lasting pain to my shoulders, neck, and back. Unfortunately, these injuries are all too common throughout a career in the fire service. I have tried cortisone shots for my back pain but ultimately decided on surgery to relieve my pain. Following surgery, the doctor prescribed pain medication during my recovery. I took one pill; it made me feel different, not like myself. Rather than continue that feeling, I chose to use alternative, evidence-based treatments instead.
Acetaminophen, ibuprofen, and naproxen sodium are over-the-counter pain relievers that may assist with pain management and are nonaddicting. If you would like to consider pain management aside from medication, some alternative treatments include physical therapy, cortisone shots to reduce inflammation in hopes of lessening pain, acupuncture, rest, stretching, meditation, natural supplements, holistic treatment, and yoga.
Meditation reduces brain activity in the part of the brain that helps identify where a pain is and its intensity. Also, studies have reported that during meditation, our bodies release high levels of endorphins, pleasure-causing neurochemicals that create feelings of well-being. Different styles of meditation also can encourage self-reflection and awareness; aid in the participant’s ability to gain a better perspective of himself; and lead to new perceptions of how to handle situations in life, including pain. As for yoga, Catherine Bushnell, PhD, scientific director of the National Center for Complementary and Integrative Health, studies how the brain processes and is affected by pain. She reports that practicing yoga has opposite effects on the gray matter of the brain than pain does. Brain imaging shows that gray matter can be altered in individuals experiencing pain, shrinking it in particular areas, and that practicing yoga can bring back some gray matter.
When Help Is Needed
As a firefighter, it can be difficult to ask for help. When you were forcing a door, clearing a window, or leading out a line, you didn’t want to be the one to ask for help. So why would it be any different when dealing with a personal issue? So what can you do when facing an issue related to taking prescription pain medication or an illegal substitute?
First, let’s get one thing clear: Asking for assistance is not a sign of weakness. As I mentioned earlier in the article, drug dependency does not discriminate. Many treatment and recovery centers are available across the United States. Recently, treatment centers with population-specific programs for firefighters have opened. One such program that serves all uniformed personnel is the Rosecrance Florian Program. It offers an excellent opportunity for lasting recovery to uniformed personnel by incorporating occupational factors and underlying co-occurring issues into the treatment process.
I remember when the Florian Program was first opened. A retired firefighter was one of the first to complete the program. While he was in treatment, another first responder was detoxing on a separate unit. He and I stopped by to see this individual going through detox. We let him know he had brothers/sisters waiting for him on the Florian unit when he completed his detox process. He was so grateful and relieved to have people there who understood him. This created a connection that is vital in the beginning stages of the recovery process.
Action
Whether you call it a crisis or an epidemic, opioid use, abuse, dependency, and deaths are reaching staggering statistics in the United States and around the world. Mental health professionals are constantly working to update our understanding and perceptions of addiction through evolving diagnoses and forms of treatment available.
Our federal government, the FDA, the Centers for Disease Control and Prevention (CDC), and many states are working to address the opioid dilemma through changes, revisions, or additions to our laws, policies, and action plans. Plans address the manufacturers, doctors, and patients, who vary from criminal justice populations to populations based on age, demographics, socioeconomic status, and professions, including pharmacists among others.
At the federal level, in March 2017, President Trump signed an Executive Order forming a President’s Commission on Combating Drug Addiction and the Opioid Crisis, with then New Jersey Governor Chris Christie as chairman. They held their first panel meeting in June. The Commission made the following immediate recommendations:
• Permit states with treatment centers with more than 16 beds to use Medicaid to finance treatment.
• Mandatory training on how to properly educate their patients for doctors who prescribe opioids.
• Issue naloxone to law enforcement officers.
• Data sharing between federal and state agencies to track patients’ opioid use.
• Collaboration with pharmaceutical companies in developing alternative pain-relieving medications.
The FDA is expanding the scope of the types of drugs for which they require drug manufacturers to offer education to doctors, clinicians, nurses, and pharmacists. They have also requested Endo Pharmaceuticals to remove the drug Opana ER, an opioid pain reliever, from the market because it is believed that the risks of taking the drug outweighs the benefits.
The CDC in 2016 created a guideline for primary care clinicians, physicians, and internists for prescribing opioids for chronic pain. They address many populations of patients and circumstances. Primarily, the guidelines are to assist in assessing appropriate treatment for pain, when to prescribe opioids, when to continue them, and when to end them.
Many states are working to make an impact on the opioid crisis. They are focusing primarily on four factors: prevention, intervention, treatment, and recovery support. Some of these states include Massachusetts, Alaska, Illinois, Ohio, and Michigan, to name a few.
As a nation, we are heading in a direction of more knowledge and action when considering pain and the use of opioids. Even with full-force efforts across the country starting today, we still have a long road ahead of us to address the damage already incurred and limiting and eventually preventing future consequences from these drugs. Let’s support one another—whether it be a friend, a family member, or a coworker—and become and remain well-informed as this effort continues.
References
https://www.nami.org/NAMI/media/NAMI-Media/Infographics/GeneralMHFacts.pdf.
http://www.cnn.com/2017/07/11/health/fda-increases-opioid-training-bn/index.html.
https://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm562401.htm.
https://teens.drugabuse.gov/blog/post/connection-between-pain-medications-and-heroin.
https://www.drugs.com/cg/opioid-withdrawal.html.
https://www.asam.org/docs/default-source/advocacy/opioid-addiction-disease-facts-figures.pdf.
https://www.hhs.gov/opioids/about-the-epidemic/index.html.
https://www.drugs.com/news/protein-involved-changes-brain-circuitry-17996.html.
https://www.nami.org/NAMI/media/NAMI-Media/Infographics/GeneralMHFacts.pdf.
https://www.whitehouse.gov/ondcp/presidents-commission/.
http://www.nj.com/politics/index.ssf/2017/07/how_christies_commission_proposed_fighting_opioid.html.
http://www.mass.gov/eohhs/feature-story/end-opioid-abuse-in-mass.html.
http://www.mass.gov/eohhs/feature-story/end-opioid-abuse-in-mass.html.
https://careertrend.com/about-4760940-much-does-firefighter-gear-weigh.html.
DANIEL DeGRYSE is a 28-year veteran of and battalion chief with the Chicago (IL) Fire Department. He was the coordinator for the Chicago Firefighters’ Union Local 2 employee assistance program. He is a member of the International Association of Fire Fighters L/EAP committee. He has a B.A. degree in psychology and is a certified substance abuse counselor and a certified EAP counselor. He created the peer support program for the Chicago Firefighters Union EAP.
RELATED
Responding to Opioid Overdoses
Pulmonary Edema Following Opioid Overdose
Narcan®: It’s Not Just for ALS Anymore
Fentanyl: Not Just Another White Powder
Engine Company EMS: Understanding Addiction and Naloxone
Opening Ceremony Keynoter Dan DeGryse Offers Straight Talk

