Orthopedic Sports Injuries in Children and Young Adults
It is another Saturday shift in the spring, and the call load has been steady. The calls have not been anything unexpected-chest pains, difficulty breathing, and fender benders. As you drive back from the hospital after dropping off your last patient, you are once again dispatched for a call. Dispatch advises you to respond to Field 4 at the local Little League for a patient who is complaining of severe lower leg pain. Dispatch also advises that the caller believes the patient has a broken leg.
Types of Injuries
Each year, more than 1.35 million youth experience a serious sports injury.1 Although concussive injuries represent a high percentage of these incidents, orthopedic injuries also occur with significant frequency and require appropriate recognition and treatment by emergency medical services (EMS) providers, especially when they occur in pediatric patients.
There are two types of sports injuries. The first is the acute injury, which occurs suddenly during sports practices or events.2 It may occur because of direct contact, such as being struck by a ball or bat, colliding with another player, or falling to the ground. It can also result from indirect contact, such as straining a muscle or spraining a joint.
The second type of sports injury is a chronic injury. (2) This occurs as a result of overuse and is becoming more frequent in pediatric and younger patients because of increased participation in year-round sports. Chronic injuries include aches, pains, and muscle strains. They result in pain and discomfort but are rarely life threatening.
It is important as an EMS provider that you appropriately assess your patient, determine the extent of the injury, and provide appropriate treatment.
As you arrive at the field, you see an approximately 12-year-old boy sitting just off first base, clutching his left ankle. He is crying and repeating that his ankle hurts. An adult, dressed as a coach, approaches you and states that the boy was running toward first base and collided with the first baseman during a play. The boy immediately fell to the ground, screaming that his ankle hurt. The coach also advises that he applied ice to the injury but has not moved the boy since the incident.
Assessment
Assessment of orthopedic injuries is important but may not point to a specific diagnosis. Signs and symptoms can give an idea of the seriousness of the injury, but, in many cases, further testing will be required to reach a definitive diagnosis.
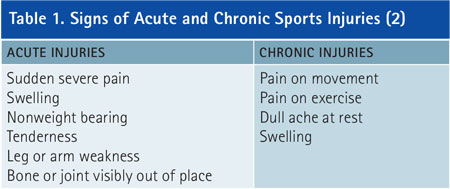
The signs and symptoms of acute vs. chronic injuries are similar; without a full assessment, you may not have a clear picture of the true extent of the injury. Table 1 lists the signs and symptoms of acute and chronic injuries. A full assessment will help you get a better picture of the injuries. Additionally, the location of the injury will determine the assessment and treatment steps.
Primary Assessment
General assessment of the pediatric and young adult orthopedic injury begins as it does with any call: scene safety and body substance isolation (standard precautions). Once you have completed these steps, rule out the need for C-spine stabilization. Few orthopedic injuries will require C-spine immobilization. Once you have assessed airway, breathing, and circulation and addressed any concerns, you can move on to your secondary assessment.
Secondary Assessment
If the injury you have been called to treat is extreme, it may be hard to avoid tunnel vision, which would cause you to focus only on the injury. Along with the standard assessment, you can also use the six Ps of limb ischemia to assess the orthopedic injury. The six Ps are as follows:
- Pain: Is there pain at the injury site? Is it sensitive to palpation?
- Pallor: Is the injured area pale, signifying compromised circulation?
- Paresthesia: Does the patient complain of numbness or tingling?
- Pulses: Is the distal pulse present?
- Paralysis: Can the patient move the affected extremity?
- Pressure: Does the patient complain of pressure in the affected area?3
The presence of any of the six Ps increases the likelihood that an orthopedic injury is compromising blood flow to the injured extremity. Hands-on assessment is important, along with talking with the patient.
Your patient assessment has revealed that your patient’s distal pulse/movement/sensation (P/M/S) is intact and that there is no additional trauma noted. Vital signs are within normal limits, although his respiratory rate is on the high side of normal. He states that his pain is a 7 on a scale of 1-10.
Treatment
The majority of orthopedic injuries you will encounter will not be life threatening, but other injuries may be, and you should treat those first. Remember that issues with the airway, breathing, and circulation are your priority when determining a treatment plan.
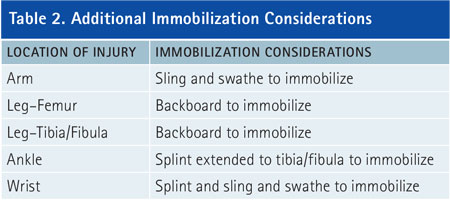
After you complete your assessment, develop your treatment plan. First, manually stabilize the injury site. Immobilization ensures that the limb does not move and prevents further injury from jagged bone ends or circulatory compromise. (3) Immobilization begins with manual stabilization of the injured extremity: Place one hand above the injury and one hand below the injury. Next, apply splints, ensuring that they extend above and below the injury. If the injury involves a joint, secure the splint to the bone above and the bone below the joint. If the injury involves a bone, the splint should immobilize the joint above and the joint below the injury site.4 Table 2 has additional information on immobilizing an extremity.
Prior to and following splint application, remember to check the P/M/S in the extremity. Note the presence or absence of each in your documentation.If the injury involves an upper extremity and does not compromise the head, neck, or spine, there may not be a need to provide spinal motion restriction. After you immobilize the extremity, you can carefully move the patient to the stretcher for transport.
With the patient’s ankle immobilized from the tibia to the foot and good P/M/S in the foot and toes, you move the stretcher closer to your patient. Using a controlled movement, you and your partner place your patient on the stretcher and load him into the ambulance. After reassuring the victim’s mother, you begin your transport.
Transport
Determine a transport destination, as always, based on multiple factors, including patient priority (high priority vs. low priority) and the hospital’s ability to treat the injuries. In the case of this pediatric patient with an orthopedic injury, the preference for transport is a hospital capable of handling both pediatric and orthopedic injuries. Follow your local transport protocols, or contact medical control for guidance in transport decision making.
During transport, providers may find an opportunity to provide additional support to the patient. Monitoring of vital signs, repeated reassessments of P/M/S, and reassessment of the immobilization device provide support and ensure that you notice any changes in the patient’s condition. Additionally, if an advanced life support provider is available, administration of analgesia such as fentanyl [1 microgram (mcg) per kilogram IV or intranasal-maximum single dose 100 mcg] or morphine (0.1 milligram per kilogram IV or subcutaneously) may assist in relieving some pain. Dosages and drugs may vary, so check your local protocols for pain control options.
You deliver your patient to the local pediatric hospital and provide a report to the nurse, after making sure the patient is settled. When you return later with another patient, the nurse advises you that your patient’s ankle was fractured and personnel are in the process of casting it.
Take Every Injury Seriously
It is important to remember that even if an orthopedic injury does not look serious, underlying structures may be severely compromised. An in-depth assessment and appropriate treatment are important to ensure you don’t worsen the injury. With the number of injuries occurring during youth sports increasing, there is a high potential you will see sports-related orthopedic injuries. Reviewing the causes, signs and symptoms, and treatments is important to providing quality care.
References
1. Healy, M. (2013, Aug 6). “Top youth sports injuries.” USA Today. Accessed November 10, 2015 from www.usatoday.com/story/news/nation/2013/08/06/injuries-athletes-kids-sports/2612429.
2. U.S. Dept of Health and Human Services: Public Health Service. (2014 Nov). “What are sports injuries?” Accessed November 10, 2015 from http://www.niams.nih.gov/Health_Info/Sports_Injuries/sports_Injuries_ff.pdf.
3. Limmer, D, Mistovich, JJ, Werman, HA, & Bastie, D. (2011, Aug 1). Transition series: Topics for the EMT – Orthopedic trauma. Accessed November 20, 2015 from http://www.emsworld.com/article/10287441/orthopedic-trauma.
4. Pollak, AN. (2013). Emergency care and transportation of the sick and injured, 10th ed. Jones and Bartlett, MA.
KAREN OWENS is the emergency operations assistant manager for the Virginia Office of EMS, where she has worked since 2001. Her duties include oversight of the emergency operations training programs including MCI management, terrorism awareness, and vehicle rescue. She has a BA in psychology and an MA in public safety leadership. She is a Virginia certified firefighter and has been a Virginia EMT-B instructor since 2002; she is the author of Incident Command for EMS (Fire Engineering, 2011).
Injuries to the Fingers and Nose
In addition to joint and extremity injuries, you may encounter injuries to the fingers, toes, or nose. Immobilize these injuries by securing the injured finger to the adjacent uninjured finger with tape or a tongue depressor.
With nasal fractures, ensure that bleeding is controlled and the airway is not compromised. Splinting is normally done using a nasal splint, most commonly at the hospital. NEVER pack a nostril with gauze unless directed to do so by medical control.
Sports Injuries in Children and Young Adults: Concussions
Fire Engineering Archives

