You’re halfway through your tour when dispatch assigns you a call that has become an all too familiar response: an unconscious male in a dorm at the local college. You and your partner go through a quick checklist: tech bag; oxygen; monitor; suction unit; and opiate overdose kit, almost reflexively.
You arrive on scene to find a group of students packed into a dorm room. You conduct a quick size-up: The scene appears safe with no apparent danger to you or your partner. You ask for the room to be cleared and discover an approximately 19-year-old male on the bed, unconscious and barely breathing. A quick clinical assessment of behavior shows a radial pulse barely palpable at 70 beats per minute (bpm), the airway appears intact and self-maintained, and breathing is agonal at seven bpm. There are no obvious signs of trauma. The skin is unremarkable with the exception of track marks on the left forearm.
 |
| (1) Naloxone overdose kit. (Photo courtesy of Mountainside Medical.) |
You and your partner make eye contact; “OD,” you both exclaim in unison. Pinpoint pupils further support your assessment. The almost rhetorical question is asked of no one in particular, “Anyone know what he took?” Silence.
As your partner assists the patient’s breathing with a bag valve mask (BVM), you assemble your opiate overdose kit, a prefilled syringe of Narcan® (naloxone) 2 millgrams (mg) in 2 milliliters (mL) and mucosal atomization device (MAD™). Your partner stops bagging, and you place the MAD in the patient’s nostril and squeeze in 1 mL of Narcan, repeating the same in the opposite nostril. Your partner resumes bagging the patient. You assemble a second syringe in case it is needed. The patient begins to regain consciousness. You keep a close eye on him and assume supportive care.
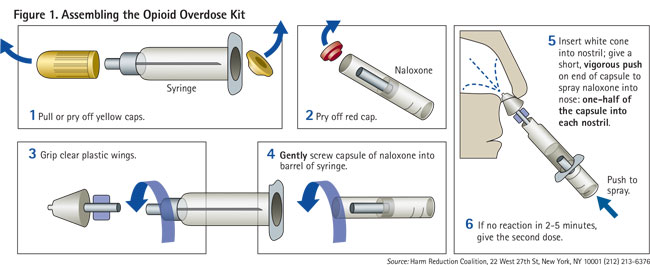
Naloxone, more commonly known as Narcan, is a medication used to reverse the effects of opioids, especially in overdose. It is a pure opioid antagonist. It works by reversing opioids-caused depression of the central nervous and respiratory systems (Table 1). The effects of naloxone last about half an hour to an hour. Multiple doses may be required, as the duration of action of most opioids is greater than that of naloxone.
Administration
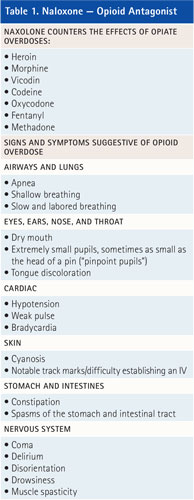
Naloxone is administered intranasally usually using an opioid overdose kit (photo 1). Naloxone can be administered by nasal spray. It can be repeated if necessary. A MAD (photo 2) device is attached to a syringe and is used to create a mist that delivers the drug to the nasal mucosa. Figure 1 illustrates how to assemble the kit.
 |
| (2) MAD. (Photo by author.) |
Nalaxone is given in 2-mg increments, dividing 1 mg into each nostril. It can be repeated every five minutes, up to a total of three doses (6 mg). If there is no response at this time, pursue alternative diagnosis and treatment.
A major advantage of the MAD device is that there is no needle involved, reducing needle sticks.
Pharmacodynamics
Naloxone has an extremely high affinity for opioid receptors in the central nervous system (CNS). Naloxone is an opioid receptor (MOR) competitive antagonist, and its rapid blockade of those receptors can produce rapid onset of withdrawal symptoms. Unlike other opioid receptor antagonists, naloxone is essentially a pure antagonist with no agonist properties. If administered in the absence of opioid use, no functional pharmacological activity occurs (except the inability of the body to combat pain naturally).
Pharmacokinetics
When administered parentally (nonorally, as in nasally), naloxone has a rapid uptake. “Narcan (naloxone) is metabolized in the liver, primarily by glucuronide conjugation with naloxone-3-glucoronide as the major metabolite. In one study, the serum half-life in adults ranged from 30 to 81 minutes (mean 64 ± 12 minutes). After an oral or intravenous dose, about 25 percent to 40 percent of the drug is excreted as metabolites in urine within six hours, about 50 percent in 24 hours and 60 percent to 70 percent in 72 hours.”1
Post-Resuscitation
Closely monitor patients for signs of improvement in respiratory function and mental status. If you observe a response, keep monitoring them closely, as the effects of naloxone may wear off before those of the opioids and the patient may require repeat dosing. Consider advance life support (ALS) intervention if warranted. Patients often refuse further medical treatment once regaining their faculties, especially if they overdose often. In general, a resuscitated patient should be transported to the hospital for further evaluation. Establish clear policies and procedures as part of the implementation of an opioid overdose program.
Final Considerations
Narcan has often been termed a “benign drug.” Although it is considered safe, administer it with caution. There are some notable side effects. Administration of naloxone to an opiate-addicted patient can trigger significant withdrawal symptoms. Side effects may include the following sudden opioid withdrawal symptoms. In someone who has been using opioids regularly, opioid withdrawal symptoms can include the following2:
- body aches or diarrhea,
- increased heart rate,
- fever,
- sweating,
- nausea or vomiting,
- nervousness,
- restlessness or irritability,
- shivering or trembling,
- stomach cramping,
- weakness, and
- increased blood pressure.
Narcan reduces constipation, and repeat doses can cause explosive diarrhea.
What If It Doesn’t Work?
Be prepared for the “what if”-what if it doesn’t work? If the patient’s clinical presentation does not improve, either the route was not effective or the patient was not experiencing an opiate overdose. If an unconscious patient fails to improve, continue to provide airway support and cardiopulmonary resuscitation if necessary. Always consider differential diagnoses when dealing with possible overdose patients. Overdose symptoms can be mimicked by stroke, diabetic ketoacidosis, hypothermia, meningitis, subdural hematoma (head injury), and syncope.
Beware of multiple drug ingestion (antidepressants, alcohol, or benzodiazepines). Although uncommon, aggressive behavior may occur. Confusion, rapid withdrawal, and the possibility of contemporaneous drug use are all important considerations when administering naloxone.
If you were to ask veteran emergency medical services providers five years ago how often they administered naloxone for a drug overdose, they would have said rarely. What was once an uncommon call has become an all too familiar occurrence today.
Resources
Narcan. Adapt Pharma, a small business, focuses on developing specialized pharmaceutical products. Its mission is to provide appropriate therapeutic options to those in need of safe, affordable, and easily accessible medication alternatives. In November 2015, the Federal Food and Drug Administration (FDA) through Fast Track Designation and Priority Review approved Narcan® Nasal Spray 4 mg for use in the United States. Narcan nasal spray is now commercially available over the counter in many states. Group purchasers, such as firefighters and other first responders, can learn more about ordering Narcan nasal spray at (844) 4-NARCAN (844-462-7226) or customerservice@adaptpharma.com.
Harm Reduction Coalition. Founded in 1993 and incorporated in 1994 by needle exchange providers, advocates, and drug users, the coalition works as an advocate for policy and public health reform in the treatment of drug overdoses. http://bit.ly/1Wvi8kv.
Video. A Naloxone video from the Ohio Attorney General’s Office is at http://www.youtube.com/watch?v=m9wgPiuCtGI.
References
1. RxList The Internet Drug Index-Narcan Clinical Pharmacology (2009). Retrieved from http://www.rxlist.com/narcan-drug/clinical-pharmacology.htm.
2. Narcan-Highlights of prescribing information (2015), page 12. Retrieved from http://www.accessdata.fda.gov/drugsatfda_docs/label/2015/208411lbl.pdf.
FRANCIS CALIFANO, BS, EMT-P, CHSP, is an emergency management coordinator for North Shore-LIJ Health System, Protective Services in Syosset, New York. He is assigned to the Emergency Management Division. He is a 30-year member of Rescue Hook & Ladder Co. #1 of Roslyn, New York. He is company safety officer and has served as captain of EMS. He has a bachelor of science degree in community services/emergency management from State University of New York, Empire State College. Califano has been a speaker at the Fire Department Instructors Conference as well as other national conferences. He is a certified hazardous materials specialist and a certified healthcare safety professional.
Fire Engineering Archives

