BY ALEX FROST, CLARA TRYON, SUSANNE D’ISABEL, AND DENISE L. SMITH
The COVID-19 pandemic disrupted the world like nothing else in this century, devastating many families and affecting every aspect of life. After three years of the pandemic, most of the U.S. population has been infected by the SARS-CoV-2 virus one or more times. The fire service has been on the front lines of the COVID-19 response and has likely suffered a higher infection rate than the population at large.
COVID-19 has killed far too many and caused severe illness for numerous others, with a varying severity of acute illness for most of us. Additionally, it has disrupted the economy, interrupted our educational system, altered operational procedures, wreaked havoc on staffing, and even caused political friction across close-knit communities.
Clearly, everyone is tired of COVID-19 and would like to move on from the disease and its disruption. Unfortunately, although most people recovered after a few weeks, many still struggle with a myriad of prolonged symptoms. When existing or new symptoms persist well past the initial infection, it is called Long COVID. Indeed, the full implications of Long COVID remain unknown in the general population and for the fire service in particular. Just as it is dangerous to not fully expose and extinguish a smoldering fire, so too is turning away from COVID-19 before we know that all the risks have been adequately attended to.
Stories from firefighters struggling with Long COVID highlight the need for the fire service to continue to pay attention to some aspects of COVID-19. The quotes below are from firefighters who completed an online survey or participated in interviews as part of a research project on Long COVID in the fire service. They have been slightly altered to protect anonymity.
“When I finally returned to work … getting back into the swing of things was extremely difficult. I hadn’t been around people in half a year, so the social aspect was mentally draining.…[W]ith the residual brain fog [and] being away from work for over half a year, I was rusty…. I did not adequately explain to my crew that I was struggling physically and emotionally. I acted like I was okay, so they became frustrated seeing me struggle with tasks I used to do easily and without thought.”
“When [I] returned to work I continued to have difficulty with headaches, exertional fatigue, heart palpitations, loss of smell, and brain fog. After 48 hour or longer shifts I would rest/sleep most of my days off. Exercise was almost impossible.”
“A young firefighter in my department who was otherwise healthy had all the variants. After dealing with COVID, he had a heart attack and now experiences significant pain and feels awful. His mental health is compromised.”
For the many firefighters who struggle with Long COVID, there is a clear sense of desperation, isolation, and pain. Frustration and concern plague those in their departments who support them. A better understanding of Long COVID in the fire service will help raise awareness among individuals suffering from an array of illnesses or conditions following their acute bout of COVID-19, and it offers an opportunity for firefighters to better appreciate the challenges that some of their fellow firefighters are facing.
Acute COVID-19 vs. Long COVID
COVID-19 is an infection caused by the SARS-CoV-2 virus and is most commonly associated with respiratory illness. As seen in Figure 1, the virus typically enters the body and binds to ACE-2 receptors in the respiratory system. The viral attack on these receptors triggers a profound immune response affecting nearly all organ systems.1, 2 During the initial, or acute, phase of COVID-19, the most common symptoms are fever or chills, shortness of breath, cough, fatigue, muscle or body aches, headache, loss of taste or smell, sore throat, diarrhea, congestion, and nausea or vomiting.3 Most individuals experience mild to moderate acute symptoms and generally recover within 10 to 20 days.4 Although rare, far too many people, including firefighters, have died of COVID-19. The National Fire Protection Association (NFPA) reports that in 2020 and 2021, COVID-19 was the leading cause of line-of-duty-deaths, claiming 143 firefighters’ lives.5,6 And, for some individuals who have endured the initial infection, COVID-19 symptoms do not completely resolve, or the infection leads to the onset of new and troublesome symptoms—a condition known as Long COVID, which is the focus of this article.
Figure 1. COVID-19 Overview
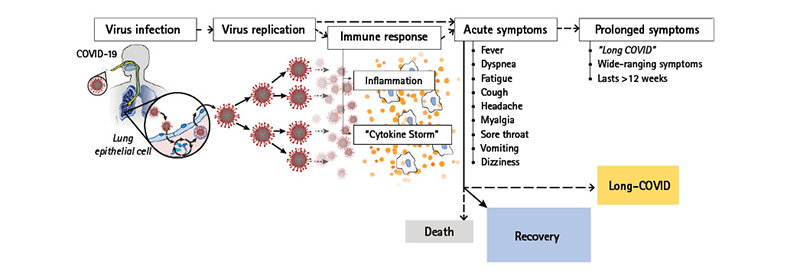
Source: Smith, et al., Skidmore College.
Long COVID, also known as Long-Haul or Post-Acute COVID Syndrome (PACS), is a potentially debilitating condition that is generally considered to occur when COVID-19 symptoms (existing symptoms or new ones) persist for more than 12 weeks.7 The full duration of Long COVID remains unknown, as some individuals have not yet returned to their prepandemic health following infection. As seen in Figure 2, the SARS-CoV-2 virus stimulates a heightened immune response that leads to inflammation across most body systems. Each body system reacts uniquely to the viral infection or the resulting inflammation to produce a wide array of burdensome and sometimes mysterious symptoms.8 Table 1 displays some of the common symptoms associated with different organ systems affected by Long COVID. Those who suffer from Long COVID may experience many, some, or just one of these symptoms and, to further complicate an already complex disease, symptoms may resolve and emerge or reemerge over time.
Figure 2. How Long COVID May Impact Firefighter Health and Safety
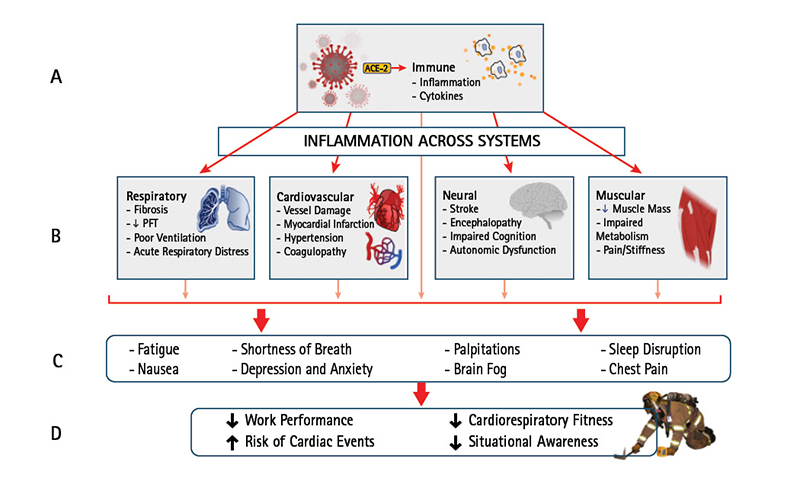
A profound immune response to the COVID-19 infection (A) leads to inflammation and complications across multiple body systems (four relevant systems presented here) (B). This results in a myriad of symptoms, many of elevated concern to firefighters (C). These symptoms can have an adverse effect on firefighter health and safety (D).
Source: Smith, et al., Skidmore College. Based on the graphic, “Long COVID: A Smoldering Issue in the Fire Service.”

* Symptoms worsen after physical/mental exertion.
+ Postural Orthostatic Tachycardia Syndrome; effects include lightheadedness upon standing.
Figure 2 outlines how Long COVID affects key body systems and how this can lead to health and safety consequences for firefighters. Changes to the respiratory, cardiovascular, neural, and muscular systems can lead to multiple conditions that increase the risk of a sudden impairment or precipitate troubling or dangerous symptoms. The changes within each system may be the result of direct effects of the virus, may reflect changes caused by chronic inflammation and associated immune responses, or may be the result of impairment in other systems.14 Furthermore, the conditions can be transitory and may resolve without long-term damage, or they may result in damage to the tissue.14 For example, firefighters may experience a temporary decrease measured during pulmonary function tests (spirometry) or they may develop fibrosis, which permanently impairs lung function.
The cardiovascular system is affected in multiple ways. Long COVID is associated with an increased prevalence of arrythmias (increasing risk for a sudden cardiac event); increased risk of hypertension (exacerbating atherosclerosis in the coronary arteries); inflammation within the blood vessels that decreases the vessels’ ability to appropriately adjust diameter;; and increased clotting potential that increases the risk of blood clots, or microthrombi, in the brain, heart, lungs, and kidneys.2,15 The neural system is also greatly affected by Long COVID. Again, this may be because of direct infection by the virus, inflammation and associated swelling, or stress associated with all other symptoms. In fact, symptoms of anxiety and depression are common neuro-psychological symptoms associated with Long COVID.1, 2 Long COVID can also impair cognitive function, a condition that is commonly called “brain fog” and reported by many patients who suffer from Long COVID.1,2 It can affect the muscular system in multiple ways but, most commonly, individuals report experiencing muscle pain and weakness (and often associated joint pain).13 In addition to muscular weakness, many long-haulers report fatigue that may be the result of decreased muscle mass or impaired metabolism within the muscle or perhaps an interaction with other systems that are necessary to deliver and use oxygen and nutrients.1
As briefly outlined in Figure 2, each system is affected in different ways, and these changes can, in turn, affect another organ system. Many of the commonly reported symptoms, such as shortness of breath, fatigue, and brain fog, may reflect impairment from multiple systems.8 In addition to resulting in myriad symptoms, the involvement of multiple organ systems leads to specific outcomes that are of great importance to the fire service, including decreased cardiorespiratory fitness, a diminished work capacity, impaired situational awareness, and an increased risk of cardiac events.
How Common Is Long COVID?
Recent data collected by the National Center for Health Statistics (NCHS) reveal that about one-third of adults reported experiencing symptoms that lasted three months or longer (Long COVID).16 Encouragingly, many people who suffer from Long COVID do see their symptoms resolve. Unfortunately, however, many continue to deal with post-COVID conditions for well over a year and, in some cases, individuals have been suffering with Long COVID for more than two years. Overall, NCHS data indicate that about 6% of U.S. adults or more than 15 million people are currently grappling with the impact of Long COVID.16 The true number of firefighters suffering from Long COVID is unknown. But, if even 6% of the fire service is struggling with Long COVID, this would suggest that more than 65,000 firefighters are impacted. Conversations with firefighters show that, oftentimes, firefighters do not reveal the symptoms they are struggling with because of a desire to be seen as fully ready for the demands of the job or because of a stigma that can be attached to the diagnosis of Long COVID.17 Because many have had COVID-19 and recovered, and because we would all like to move beyond the pandemic, many people with Long COVID feel like others are dismissive of their symptoms/conditions. This can make a firefighter who is experiencing post-COVID-19 complications less likely to talk about and address issues that are impacting work and life.
Why Do Some People Get Long COVID?
There is not a good way to know or predict who will experience Long COVID. However, studies have identified certain factors that increase the risk of suffering Long COVID. These include the following:
- A severe initial COVID-19 infection as evidenced by being hospitalized and/or in an intensive care unit, suffering more than five symptoms, or experiencing multisystem inflammatory syndrome during/after acute illness.9,10,14,18
- Having certain underlying conditions such as diabetes, asthma, or obesity.8,10,18,19
- Being female.8,10,14,18,19
- Not being vaccinated.9,18,20
Although these risk factors increase the chance of experiencing Long COVID, many who fall into these categories do not go on to develop Long COVID and many who fall outside of these parameters do, in fact, develop Long COVID. Researchers are still working to understand who is at risk of suffering from Long COVID and why. While many of the risk factors currently identified are either difficult to impact or not modifiable at all, vaccination represents a possible avenue for mitigation. Currently, vaccination is the most effective way to reduce the severity of COVID-19 and, as seen above, severity of acute infection is closely linked to increased risk of developing Long COVID.18,20 Furthermore, a systematic review of multiple studies found a 29% lower risk of Long COVID in vaccinated vs. unvaccinated individuals.21
Diagnosing and Treating Long COVID
Because Long COVID encompasses a variety of symptoms, there is no one diagnostic test for it. Routine clinical tests, including those used during occupational medical evaluations, often do not detect abnormalities. Furthermore, symptoms may have waves of improving and then regressing, which complicates diagnosis. Many health care providers are not fully aware of the complexities and nuances of Long COVID. All these factors make diagnosing and treating Long COVID difficult and frustrating.
Treatment for Long COVID is focused on addressing symptoms and specific conditions associated with it. As such, the best course of treatment requires a personalized approach tailored to the unique constellation of an individual’s ongoing symptoms. The Centers for Disease Control and Prevention provides guidance on how to effectively prepare for and communicate with your health care provider to facilitate diagnosis and treatment (www.cdc.gov/coronavirus/2019-ncov/long-term-effects/post-covid-appointment/index.html). In addition, because symptoms are often difficult to treat and are so varied, clinics that bring together specialists who focus on Long COVID have emerged, though they are often clustered in urban/high population areas. Grassroots organizations such as the C-19 Longhauler Advocacy Project have resources online and on their Web sites and social media outlets to direct individuals to resources including post-COVID-19 specialty clinics and Long COVID support groups.
Challenges for the Fire Service
The fire service has faced many challenges in the course of the pandemic. In fact, given the evolving nature of the virus, the acute illness continues to be a challenge in many parts of the country. For Long COVID, specific issues still need to be addressed. It is often difficult to know when a firefighter is well enough to return to work, how to provide appropriate support to department members who are suffering from prolonged symptoms, and how to meet the operational needs of the department given the number of firefighters who may be out because of acute infection or chronic symptoms. A different challenge may arise because many firefighters may push themselves to return to work while they are still experiencing symptoms that may create safety risks, such as suffering severe work-induced fatigue during emergency operations. Similarly, a firefighter who returns to firefighting while still combating the effects of COVID-19 may be at risk of a health emergency during operations, such as suffering a clot formation that leads to a stroke or heart attack.
Long COVID Research
There is an enormous need for research on Long COVID. The National Institutes of Health has devoted a tremendous amount of resources toward research to better understand the causes and consequences of Long COVID. Unfortunately, there is very little research specific to the fire service. But there is an Assistance to Firefighters Grant-funded project devoted to better understanding the ongoing challenges of Long COVID in the fire service. Continuing the Fight Against COVID Together (C-FACT) is led by Skidmore College investigators in collaboration with researchers, occupational health providers, and fire service leaders across the country. The primary goals of that project are to gather relevant information from scientific/medical literature, occupational health providers, and firefighters; develop high-quality resources that educate specific groups about the risks; and distribute educational resources through multiple channels. Input from firefighters who are experiencing prolonged symptoms is critical in this process. If you are a firefighter with Long COVID symptoms, please use the QR code at right to help the fire service respond to this issue. If you know firefighters who are experiencing prolonged symptoms, please forward the QR to them.


Because of sleep interruptions and irregular schedules, most firefighters experience fatigue; however, for those struggling with Long COVID, fatigue can take the form of debilitating exhaustion. While a firefighter may be able to manage less-exacting routines at the station, there is a concern that firefighters may not have the reserve necessary to adequately meet the strenuous nature of emergency operations. Unlike traditional jobs, firefighting requires sustained energy. Firefighting also demands focus, and fatigue, along with brain fog, can interfere with the situational awareness necessary to make critical decisions in the field. This can lead to dangerous, potentially life-threatening situations for the firefighter and his team.
Accordingly, the decision of when to return to work should be well considered. It may be wise to make sure the occupational physician is working with the treating physician to ensure that the treating physician understands the unique job tasks of firefighting. Firefighters, by nature, are action-oriented and may tend to rush the recovery process. Unfortunately, for many people, the recovery from Long COVID is slow! It can be mentally and physically taxing, but individuals dealing with a wide range of Long COVID challenges must give themselves the time they need to recover.
Firefighters and fire departments continue to face ongoing challenges from the pandemic, including how to effectively deal with the impact of Long COVID. Unfortunately, there is a lack of research specific to the long-term effects of COVID-19 on the fire service (see sidebar, “Long COVID Research”). Becoming aware of Long COVID symptoms and recognizing its impact are the first steps to successfully meeting the challenges individual firefighters and the fire service face.
Firefighters are great at taking care of each other on the fireground and during times of loss. They should embrace this defining feature of their culture and watch for signs and symptoms of Long COVID among themselves and each other. Also, they should support each other during this difficult illness by helping to identify sources of appropriate medical support for firefighters who are struggling, as well as providing ongoing encouragement and support. The full effects of the COVID-19 pandemic are still unfolding, and it will take the strength, resilience, and compassion inherent in the fire service to navigate these unique and challenging circumstances.
Authors’ note: We thank the firefighters who have responded to our survey and spoken with us to help our research team better understand the impact of Long COVID on firefighters. We also acknowledge the expertise of Dr. Wesley Lefferts in designing our graphics. We thank Chief Matthew Tobia of the Harrisonburg (VA) Fire Department and Chief (Ret.) Craig Haigh of the Hanover Park (IL) Fire Department for their careful review and insightful comments on our draft manuscript.
ENDNOTES
1. Crook H, Raza S, Nowell J, Young M, Edison P. Long covid—mechanisms, risk factors, and management. BMJ. 2021;374:n1648. https://bit.ly/3LP9Y63.
2. Raman B, Bluemke DA, Lüscher TF, Neubauer S. Long COVID: Post-acute sequelae of COVID-19 with a cardiovascular focus. Eur Heart J. 2022;43(11):1157–1172. https://bit.ly/3JJVUYB.
3. Centers for Disease Control and Prevention Web site [Internet]. Symptoms of COVID-19. Atlanta (GA): US Department of Health and Human Services. [revised 2022 Oct 26; cited 2023 Feb 1]. Available from: https://bit.ly/3FToF43.
4. Centers for Disease Control and Prevention Web site [Internet]. Ending isolation and precautions for people with COVID-19: Interim guidance. Atlanta (GA): US Department of Health and Human Services. [revised 2022 Aug 31; cited 2023 Feb 3]. Available from: https://bit.ly/3JKciIC.
5. Fahy RF, Petrillo JT. Firefighter fatalities in the US in 2020. Quincy (MA): National Fire Protection Association; 2021. Available at: https://bit.ly/3nanGG6.
6. Fahy RF, Petrillo JT. Firefighter fatalities in the US in 2021. Quincy (MA): National Fire Protection Association; 2022. Available at: https://bit.ly/32u220L.
7. Venkatesan P. NICE guideline on long COVID. Lancet Respir Med. 2021;9(2):129. https://bit.ly/3K62DgY.
8. Davis HE, McCorkell L, Vogel JM, Topol EJ. Long COVID: major findings, mechanisms and recommendations. Nat Rev Microbiol. 2023;13:1–14. Epub ahead of print. https://doi.org/10.1038/s41579-022-00846-2.
9. Centers for Disease Control and Prevention Web site [Internet]. Long COVID or post-COVID conditions. Atlanta (GA): US Department of Health and Human Services. [revised 2022 Dec 16; cited 2023 Feb 1]. Available from: https://bit.ly/40ugWlv..
10. Nittas V, Gao M, West EA, et al. Long COVID through a public health lens: An umbrella review. Public Health Rev. 2022;43:1604501. https://bit.ly/3JID9oH.
11. Garg M, Maralakunte M, Garg S, et al. The conundrum of “long-COVID-19”: A narrative review. Int J Gen Med. 2021;14:2491-2506. https://bit.ly/3lFxp73.
12. National Academies of Sciences, Engineering, and Medicine. Long COVID: Examining long-term health effects of COVID-19 and implications for the Social Security Administration: Proceedings of a workshop. 2022. Washington, DC: The National Academies Press. https://bit.ly/40g6v4A.
13. Groff D, Sun A, Ssentongo AE, et al. Short-term and long-term rates of postacute sequelae of SARS-CoV-2 infection: A systematic review. JAMA Netw Open. 2021;4(10):e2128568. https://bit.ly/3LKzh9f.
14. Yong SJ. Long COVID or post-COVID-19 syndrome: putative pathophysiology, risk factors, and treatments. Infect Dis (Lond). 2021;53(10):737-754. https://bit.ly/42Gif1Q.
15. Xie Y, Xu E, Bowe B, Al-Aly Z. Long-term cardiovascular outcomes of COVID-19. Nat Med. 2022;28(3):583-590. https://bit.ly/3lFNDgy.
16. Centers for Disease Control and Prevention, National Center for Health Statistics Web site [Internet]. U.S. Census Bureau, Household Pulse Survey, 2022–2023. Long COVID. [revised 2023 Jan 25; cited 2023 Feb 1]. Generated interactively from: https://bit.ly/3FR5cRH.
17. Pantelic M, Ziauddeen N, Boyes M, O’Hara ME, Hastie C, Alwan NA. Long Covid stigma: Estimating burden and validating scale in a UK-based sample. PLoS One. 2022;17(11):e0277317. https://bit.ly/40hRoru.
18. Koc HC, Xiao J, Liu W, Li Y, Chen G. Long COVID and its management. Int J Biol Sci. 2022;18(12):4768-4780. https://bit.ly/3Z96vlK.
19. Subramanian A, Nirantharakumar K, Hughes S, et al. Symptoms and risk factors for long COVID in non-hospitalized adults. Nat Med. 2022;28(8):1706-1714. https://bit.ly/42G670Q.
20. Antonelli M, Penfold RS, Merino J, et al. Risk factors and disease profile of post-vaccination SARS-CoV-2 infection in UK users of the COVID Symptom Study app: a prospective, community-based, nested, case-control study. Lancet Infect Dis. 2022;22(1):43-55. https://bit.ly/3FKZ4Kr.
21. Gao P, Liu J, Liu M. Effect of COVID-19 vaccines on reducing the risk of Long COVID in the real world: A systematic review and meta-analysis. Int J Environ Res Public Health. 2022;19(19):12422. https://bit.ly/3nnEgCr.
ALEX FROST is a student in the Health and Human Physiological Sciences Department at Skidmore College in Saratoga Springs, New York. She is studying the long-term effects of COVID-19 for her senior thesis.
CLARA TRYON is a project manager for a FEMA-AFG project focused on the impact of Long COVID on the fire service through the First Responder Health and Safety Laboratory at Skidmore College in Saratoga Springs, New York.
SUSANNE D’ISABEL is a project manager for a FEMA-AFG project focused on firefighter health and safety through the First Responder Health and Safety Laboratory at Skidmore College in Saratoga Springs, New York.
DENISE L. SMITH is a professor of health and human physiological sciences and director of the First Responder Health and Safety Laboratory at Skidmore College in Saratoga Springs, New York; is a senior research scientist at the University of Illinois Fire Service Institute; and has conducted more than 40 firefighter fatality investigations for the NIOSH Fire Fighter Fatality Investigation and Prevention program.

