By FRED HAAS
Providing care to a patient suffering the effects of chemical exposure presents a challenge to emergency medical responders. Symptoms of exposure are often vague, masking a potential illness. Patients may require decontamination, a skill that is not performed routinely. The treatment of some chemical exposures involves antidotes not found in the everyday emergency medical services (EMS) medical kit. A ToxMedic program may benefit departments as they address serving these patients.
ToxMedics are EMS providers who receive additional training in medical care of hazardous materials exposure. The amount and type of training will depend on your service’s current staffing types and levels. For example, a fire service EMS provider may already have baseline hazmat training to the level of technician. He will already be familiar with risk assessment, routes of exposure, personal protective equipment (PPE), and decontamination. Additional training in toxicology, physiology of chemical exposure, and use of antidote therapy will be required. On the other hand, a system that performs primarily EMS operations will most likely also require training in hazmat response techniques not covered in traditional EMS training.
There are many goals behind establishing a ToxMedic program; of primary importance is responder safety. A ToxMedic works closely with the safety officer to ensure that risks are identified and minimized. In addition, responders are informed about possible chemical symptoms to quickly recognize exposure. ToxMedics work in the “warm zone,” triaging patients entering the decontamination process. They quickly identify those exposed and symptomatic to direct urgent decontamination and treatment. Finally, ToxMedics provide the medical support to the hazmat response team. This can include medical monitoring and surveillance, rehab assessment, and treatment of team members suffering illness or injury. Although ToxMedics are prepared to care for civilian patients exposed to chemicals, the same antidotes used on patients will also benefit responders who become affected while operating on scene. This concept is the most valuable reason to implement a ToxMedic program in your department.
The first step a department should take in determining the need for a ToxMedic program is to conduct a needs assessment. Are there medications that do not exist under your current EMS standard of care? What level of hazmat experience do your EMS responders possess? What are the chemical risks in your community that require special medical treatment considerations? Many existing programs were established with the risk of chemical terrorism in mind. Although this unknown risk is something for which you need to prepare, remember that the treatment of many chemical weapons of mass destruction will be similar to treatment of industrial chemical exposures. A ToxMedic program will be beneficial in high-profile events as well as in many of the common operations you face every day.
Answering the above questions will require some research and outreach. Your department will benefit from identifying key stakeholders in the community who can provide information and resources to help implement your program. An important first contact is the department’s medical director or the local authority that regulates EMS responders. Determine what medical resources already exist. Will you need to make any changes to the EMS scope of practice to allow for new antidote medications? Hospitals may already have preparedness efforts in place; EMS can partner to extend those resources to the incident scene.
State, county, and local emergency management agencies (EMAs) are also important allies to help you to not only identify local needs but also provide assistance in locating resources necessary to establish a program. A community’s local emergency planning committee is a source of information to determine what chemicals are present in your region. That list may identify specific risks based on amounts present or medical impact. Using that chemical inventory will allow your planners to evaluate the need for any special antidotes.
Also, don’t forget your own department resources. Review incident reports on hazmat responses to determine what chemicals your department routinely sees. Your preplanning can be used to identify chemical risks. While making contacts to conduct site surveys, assess existing treatment capabilities at that location. Some industries have medical treatment facilities and may already have antidotes available. In these situations, the chemical facility will initiate care. Protocols and policies will be required to permit EMS responders to continue this care during transport.
Logistically, there are many deployment models to best meet your department’s needs. Each EMS unit could be outfitted with equipment and antidotes to ensure that a ToxMedic unit will be present at all incidents. This model presents challenges when stocking a large amount of seldom-used medications. Expiration dates coupled with nonuse means frequently swapping out outdated medications; this results in increased costs.
A second deployment option would be to equip special units only. Perhaps the department has special operations vehicles that respond to incidents involving hazardous materials. Stocking a limited number of units lowers costs. However, consider the possibility that one of these special vehicles may be assigned elsewhere and may not be available for a needed response.
In addition to deploying the medications, another concern is your department’s personnel who will train to be part of this program. Without a doubt, training is the biggest hurdle your department will encounter in establishing a ToxMedic program. Training hours, backfill to provide coverage, course materials, and tuition all add up quickly. As with the deployment of antidotes, there are many options to consider when training your medics.
A smaller department may benefit from training all its personnel. ToxMedic training can be accomplished through the department’s continuing education efforts. Many of the training programs available are worth varying hours of credit for most states’ recertification processes. By training everyone, it is easy to ensure that a ToxMedic will be on the scene of any toxic exposure.
In a larger department, training everyone may not be practical, financially and for skill retention. These departments may opt to train a small cadre of providers who staff units typically assigned to hazmat incidents. This plan has the advantage where the department can invest training resources to a small number of medics, providing more intense training.
Before reviewing training, review an example of how one department developed its ToxMedic program. Sussex County (DE) Emergency Medical Services (SCEMS) is a third-party advanced life support (ALS) service. EMS is provided in cooperation with 21 basic life support ambulances operated by volunteer fire departments throughout the county. SCEMS staffs eight dual-medic, nontransport ALS units along with two district supervisors on duty each shift. Initially, each medic truck had a fully stocked “ToxBox” (photo 1) as part of its equipment supply. ToxBox contents are listed in Table 1.
 |
| (1) Photos by author. |
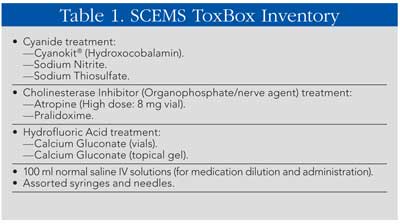
Delaware Office of EMS medical directors (with strong involvement by state ALS providers) developed ToxMedic protocols to address the needs of the state’s industrial base as well as to prepare for chemical terrorism. Each county ALS service is free to implement the program in a manner that best meets its individual needs. SCEMS initially trained 20 paramedics—all members of the Hazardous Materials Medical Response Team. ToxMedics were split among four shifts. Initially, this worked well, but as shift assignments changed and promotions occurred, keeping the roster balanced among four shifts proved challenging. Also, as previously mentioned, stocking and maintaining 10 ToxBoxes full of antidotes presented its own challenge.
To address these challenges, SCEMS recently changed its deployment model to remove the antidotes from the standard field units. This allowed it to maintain better stocked kits on the two supervisor units. An EMS supervisor routinely will be present on the scene of any major incident, including hazmat. This system has been more efficient and just as effective. Your challenge will be to set up a deployment method that bests suits your department and community.
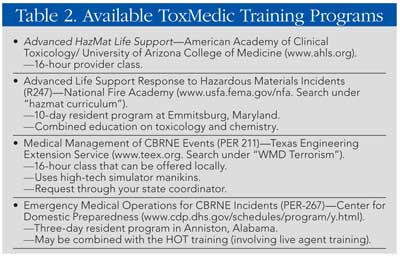
There are many existing training programs to consider when educating your medics; Table 2 lists just a few. Departments should research these training programs to determine which works best to meet their needs; include your medical director and those developing the care protocols in this decision. Some of these programs can be run for no cost through preparedness grants. Contact your local EMA for assistance.
EMS providers in nonfire based departments may require additional hazmat training. Technician level training gives responders experience in scene size-up, research, decontamination, and PPE. Although the ToxMedic’s primary role is dealing with safety and medicine, technician-level training provides the understanding of what other responders on the scene are dealing with. SCEMS ToxMedics receive a full technician class in addition to the Advanced Haz Mat Life Support class.
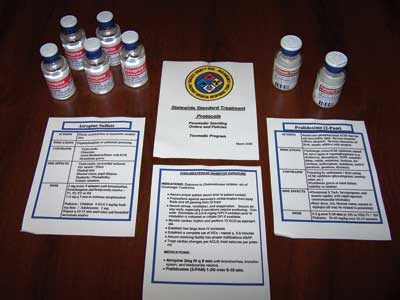
Continuing medical education is a major component of the ToxMedic program. Annual refresher training is required to maintain technician certification. Because the medications and protocols are used infrequently, all ToxMedics should receive updates and protocol reviews regularly. Equipment can be organized to aid in remembering protocols. In the SCEMS ToxBox is a pocket guide that lists each tox protocol and includes antidote information. Guides are color coded to match protocols and antidotes. For example, the anticholinergic treatment protocol is colored blue. The vials of atropine and pralidoxime used to treat anticholinergic exposures have blue tape around them, making them readily identifiable (photo 2).
Frequent drilling will not only refresh toxicology and treatment knowledge, but it will also identify areas where standard treatments may not work in a hazmat environment. For example, the majority of antidotes are administered intravenously. As paramedics drill, they quickly identify that tactile skills, such as establishing an intravenous (IV) line, are difficult to perform while wearing high levels of hazmat PPE (photo 3). As an alternative, departments may look to other routes for medication access such as intraosseous (IO) devices (photo 4). The majority of antidotes may be administered through an IO if an IV cannot be established.


Airway management is one of the key interventions in many toxic exposures. An airway protected early provides adequate ventilation to a patient who would otherwise succumb to his injuries. Performing endotracheal intubation while wearing PPE will present another challenge to the paramedic (photo 5). The use of dual-lumen airways or other devices that do not require airway visualization may be important supplements for the ToxMedics (photo 6).


A ToxMedic program is a valuable addition to a department’s hazardous materials incident response. It can effectively treat patients exposed to toxic chemicals using specialized antidotes and, more importantly, it can be an important asset to ensure the health and safety of your firefighters and emergency responders.
FRED HAAS, NREMTP, is the paramedic district supervisor of the Sussex County (DE) Emergency Medical Services (SCEMS). He is a ToxMedic and hazardous materials technician with the SCEMS’s hazardous materials medical response team. Haas is also the emergency preparedness coordinator in the Delaware Office of Emergency Medical Services and the EMS captain for the Selbyville (DE) Volunteer Fire Company.
Fred Haas will present “Implementing a ToxMedic Program in Your Department” on Friday, April 11, 10:30 a.m.-12:15 p.m., at FDIC 2014 in Indianapolis.
Fire Engineering Archives

