EMS Growth in Montgomery County
FEATURES
Throughout the United States, there is a wide variety of techniques used to supply emergency medical services. These techniques vary from the fully paid operation of ambulances and mobile intensive care units to an all-volunteer delivery system for emergency medical services. In Montgomery County, Md., we use a combination of career and volunteer personnel to man our ambulances and mobile intensive care units.
Montgomery County, a Maryland suburb of Washington, D. C., consists of approximately 516 square miles with a population of almost 600,000. The fire and rescue services are provided by 16 independent fire departments and two rescue squads. The activities of these 18 departments are governed by the Montgomery County Fire Board, composed of two members of each of the departments. Within the county government there was created in 1973 a Department of Fire and Rescue Services, an agency which provides coordinated, centralized supporting services to the fire departments and rescue squads. These services include communications, training, fire prevention enforcement, education, and investigation, administrative services and emergency medical services.
The Montgomery County Fire and Rescue Services responded to almost 48,000 incidents in 1977 with approximately 63 percent of these incidents being emergency medical or rescue related. These incidents were managed by 43 ambulances, seven mobile intensive care units, and six heavy rescue trucks.
Start of program
Citizens of Montgomery County were the beneficiaries of a pilot project for pre-hospital advanced life support administered by the Montgomery County Chapter of the American Heart Association. The fire and rescue services cooperated with this program and provided the dispatching service. This program clearly demonstrated the value of pre-hospital emergency care and stabilization prior to transport to a hospital. During the 2 1/2 years this program operated (1970-1973), a training program for paramedics was developed and implemented. There were 40 paramedics who were trained to assist the nursing staff on the unit.
When the funding for this program was exhausted, a plan for continuing this type of EMS service was prepared. The objectives of the plan were to:
- Complement the existing ambulance service, composed of 38 ambulances, with three mobile intensive care units (MICU). These units were to be staffed by certified paramedic personnel capable of providing on the scene treatment and supportive care en route to the hospital.
- Provide a communications network that would enable the paramedic to have verbal communications with and transmit EKG to the hospital where the patient was to be transported.
- Maintain and advance the training and skills of paramedic personnel by assuming the responsibility for the training from the Heart Association.
- Maximize the use of existing personnel and resources in implementing and maintaining an EMS program.
EMS officer appointed
To help accomplish these objectives, a position of emergency medical services officer was created within the Department of Fire and Rescue Services. The position was filled by the head nurse of the former heartmobile who had initiated the paramedic training program. It took a year of planning and preparation until the first two mobile intensive care units (MICUs) were placed in service. Let’s review the EMS system that evolved from this period of time by examining the EMS components of the Montgomery County Fire and Rescue Services.


Critical Care Incident Categories
Heart attack
Trouble breathing
Unconscious person
Chest pain
Possible DOA
Automobile accident with person trapped
Allergic reactions
Drownings
Electrocutions
Serious burn injuries
Gunshot or stab wound to head or trunk of body
Second or greater alarm fires in nursing homes and similar institutions
“Disaster” incidents
At the discretion of the communications supervisor on incidents when serious illness or injury is suspected
The initial two MICUs were placed in the two rescue squads in Bethesda and Wheaton. These locations were selected because the squads had the largest number of emergency care personnel to staff the units and were located in densely populated areas. A third unit was placed in service in Rockville a year later when additional paramedics were trained. This unit served the upper mid-county area, which was a considerable distance from the four community hospitals.
These MICUs were dispatched on all critical care category incidents within a 10-minute response from their location. In areas outside their station’s first-due area, the closest ambulance to the incident was also sent to provide support until the MICU could arrive. In situations when the EMT-A on the ambulance assessed that the patient’s condition was not critical or unstable, the MICU was placed back in service. If the EMT-A was uncertain, the ambulance crew waited for the MICU to have the paramedic examine the patient and decide, in consultation with a physician via radio, which unit would be used to treat and transport.
Full function unit
In 1975, a fourth MICU was placed in service in the Hillandale Volunteer Fire Department. This unit was placed in service as a “full function” MICU. It was dispatched on all emergency care and fire-related incidents in its station’s first-due area and all critical care incidents within a 10-minute response area.
At the same time Medic 4 was placed in service, the equipment on the ambulances in the county was upgraded. In departments with paramedics, a kit (referred to as a paramedic kit), was secured aboard the ambulances. The medic kits contained intravenous supplies and noncardiac emergency drugs to be used by paramedics when they were riding ambulances in departments without MICUs. The locks on the medic kits were all keyed alike and only paramedics had access to the kits.
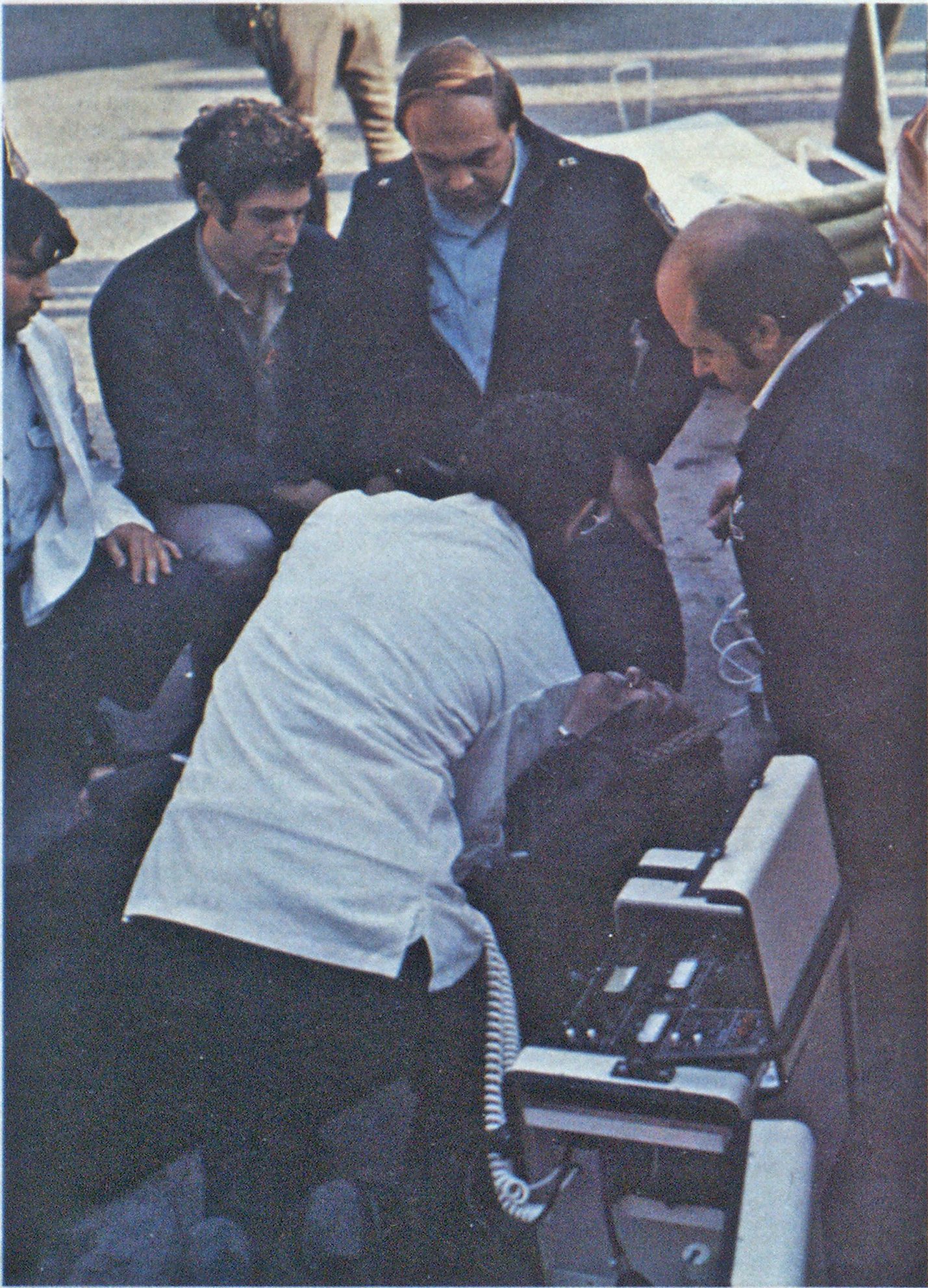
When ambulances were dispatched with an MICU, the paramedic on the ambulance initiated treatment on critical care patients or resuscitations while awaiting the arrival of the MICU with its monitoring equipment and additional drugs. In certain critical situations not involving cardiac complications, the paramedic on the medic-ambulance was able to provide all the advanced support treatment required and the MICU was left available to respond to cardiac and resuscitation incidents.
Three additional MICUs were in service in 1977 and 1978 and operated as full function units like Medic 4. Of the 38 ambulances in the county, 37 were equipped with medic kits.
Service record
In 1977, the mobile intensive care units responded to approximately 8500 incidents. The units treated, on an average, 43 percent of the patients seen (administered IV therapy and/or medications). In 1977, 355 resuscitations were attempted, 78 of which were considered successful. It’s interesting to note that while the number of MICUs has increased, almost one a year, and the number of incidents to which MICUs have responded has tripled since 1974, the number of successful resuscitations remains almost constant at approximately 80 per year.
Statistics have been collected and maintained to determine the value of having medic kits on ambulances. During 1977, paramedics responded on 6200 ambulance incidents, both alone and in conjunction with MICUs. Only 204 patients required treatment by paramedics staffing these units. While the use of this additional service has not been remarkable, the cost is minimal ($40 for kit and cost of initial drug supply) and it does result in less time on the scene by the MICU staff, since treat ment is often initiated by the paramedic on the ambulance. In multiple victim incidents the extra medic kits are useful when more than one paramedic is on the scene, since it allows functioning independently on different patients.
All the MICUs and 75 percent of the ambulances in Montgomery County meet federal specifications. The ambulances which do not are due to be replaced within the next few years and are primarily used as reserve pieces. The emergency care vehicles are equipped to meet the Maryland State Firemen’s Association’s minimum standards as well as those of the American College of Orthopedic Surgeons.
When the initial MICUs were placed in service, the four community hospitals were requested to restock the IV and medical supplies for the units on a charge-back procedure to the patients. The procedure worked well and was extended to the ambulances with medic kits. Eventually, all emergency care vehicles will be allowed to restock items that are chargeable to the patient by using a form approved by the hospitals. The hospitals have found that their unaccountable losses of supplies have decreased, so both fire and rescue and the hospitals have benefited.
Montgomery County Fire Board regulations require that every ambulance be minimally staffed by an EMT-A serving as patient attendant and a driver. The MICUs are required to be staffed with a paramedic and two EMT-As (one serving as driver). All EMT-As serving on the MICUs are required to take a six-hour orientation program prior to being assigned.
MICU Drug List
* Adrenalin 1:2000 and 1:10,000 Aramine
Atropine
Calcium gluconate
* Benadryl
Demerol
Dopamine
Isuprel
Lasix
Morphine sulfate
* Narcan
* Sodium bicarbonate * Valium
* Drutts included in medic kit in ambulances
Staffing patterns of career and volunteer personnel vary, although in most departments weekday staffing of ambulances and MICUs is primarily with career personnel. In the evenings and on weekends, the units are staffed by volunteers. Career paramedics receive a 5 percent pay differential when assigned to an ambulance and a 10 percent differential.
The Montgomery County Department of Fire and Rescue Services adopted a career development plan which has a separate career ladder in emergency medical services. The advantages of this career structure are:
- It enhances recruitment of highcaliber personnel into emergency medical services.
- Experienced emergency care personnel don’t have to leave emergency medical services to be promoted.
- Operational emergency care personnel are supervised by officers with knowledge and experience in the specialty.
Training program
Most of the emergency care and rescue training is conducted at the Fire and Rescue Training Academy in Rockville. All training is offered both during the day, evening and weekends to accommodate both career and volunteer personnel. EMT-A basic and refresher, paramedic basic and continuing education, rescue courses and CPR instructor courses are taught and/or coordinated by the EMS section of the Department of Fire and Rescue Services.
The EMT-A course is 84 hours and follows the Department of Transportation and Maryland Fire and Rescue Institute guidelines. Certification of EMT-As is performed by the Maryland Institutes of Emergency Medical Services, based on written and practical examinations. This fall, an additional nine hours will be added to the EMT-A courses in Montgomery County to teach insertion of the esophageal obturator airway, application of the medical antishock trousers and MICU orientation.
EMT-As are required to recertify every three years by taking a 21-hour refresher course. Because of the large number needing the training and the need to have fire/rescue personnel available for emergency response, the refresher training is taught in the fire stations. Each year approximately eight EMT-A basic courses and 15 refresher courses are conducted. There are currently 1200 certified EMT-As in Montgomery County.
The paramedic training consists of 200 hours of didactic and clinical experience. While the lectures and laboratory sessions are held at the training academy, clinical experience is obtained with the IV therapy departments, coronary care units, and emergency departments of the county hospitals and also on the MICUs. Upon successful completion of the paramedic course, the candidates must pass a written certification examination administered by the Maryland State Board of Medical Examiners.
Following state certification, the paramedic serves a six-weeks internship under an experienced paramedic prior to an oral structured interview before representatives of the EMS committee of the Montgomery County Medical Society. If the physicians do not feel confident that the candidate is competent to serve as a paramedic, then the internship is extended another three months. Following the extension, the candidate must again be interviewed by physicians from the medical society and then the candidate is either approved or dropped from the program.
Recertification
Paramedics are recertified annually, based upon meeting the following requirements:
- Riding a minimum of 24 hours per month on the MICUs.
- Attending four continuing education workshops (about 32 hours).
- Meeting minimum skill requirements as set forth in the Maryland State Cardiac Rescue Technician Standards. Paramedics failing to meet these minimum skill requirements in the field can be certified in the skills if they perform them before a paramedic instructor and are found competent.
Because of the stringent requirements for achieving and maintaining paramedic status, there is about a 25 percent turnover in the paramedic course. There are, to date, approximately 135 paramedics staffing our seven MICUs.
All emergency care and fire apparatus is centrally dispatched by the communications section of the Department of Fire and Rescue Services at the Emergency Operations Center in Rockville. In 1974, all emergency care vehicles were made capable of direct voice communication with all four community hospitals by putting crystals in the VHF radios already in the ambulances for the HEAR (155.340 MHz) frequency. Radio heads and hand sets were installed in each patient compartment to facilitate direct communication with the hospital emergency departments.
Telemetry capability
The MICUs were equipped with UHF radios which not only provided for voice communication with the hospitals, but also allowed for EKG telemetry. Since no other jurisdictions in the area were using the UHF-EMS frequencies at that time, a med channel was assigned to each of the hospitals.
In 1977, the State of Maryland and other jurisdictions in the Washington Metropolitan Area developed advanced life support programs necessitating coordination of the UHF frequencies. At that time, the Montgomery County system was assigned one primary and two secondary med channels to use for radio telemetry and voice communications with the hospitals. An EMS communications console was installed in the Emergency Operations Center to coordinate EMS communications with the emergency departments. Because of the limited availability of the UHF frequencies, procedures were developed whereby the UHF frequencies are used primarily for incidents requiring telemetry. A telephone patch and VHF communications are used as alternatives to the UHF system for the management of non-cardiac related incidents.
On all medical emergencies, medical direction is provided by the hospital to which the patient is to be transported. In 1978, Suburban Hospital in Bethesda was designated the regional trauma center for Montgomery County, and at that time, communication protocols were revised, requiring that communications and medical directions for multiple and acute trauma be provided by Suburban Hospital.
Division of responsibilities
Operational command and supervision of emergency care personnel and vehicles is provided by the individual fire departments and rescue squads in the county. The overall authority and responsibility for maintenance, upgrading and evaluation of the operational aspects of the EMS program rests with the Montgomery County Fire Board through its emergency medical services committee. The committee and its chairman are appointed annually by the chairman of the board. The EMS committee represents both career and volunteer personnel from various departments comprising the Montgomery County Fire and Rescue Services. The duties and responsibilities of this committee consists of:


- Establishing regulations of conduct and procedures for Montgomery County Fire and Rescue Services emergency care personnel consistent with the state law, and regulations of the Board of Medical Examiners of Maryland, Maryland Institute of EMS, Montgomery County Medical Society and other appropriate agencies.
- Defining the nature and scope of training for emergency care personnel.
- Establishing and maintaining a system of supervision and evaluation of emergency care personnel.
- Removing from paramedic status any paramedic failing to maintain standards in proficiency.
- Establishing vehicle and equipment standards for emergency care apparatus.
Within the Department of Fire and Rescue Services, the Emergency Medical Services Section provides staff support to the EMS committee and its work groups. In addition to this, personnel of the EMS section maintain liaison with representatives from each of the departments and Montgomery County hospitals and the Medical Society. Among other duties and responsibilities, the EMS section is empowered to:
- Develop and maintain training programs for all emergency care personnel.
- Maintain quality assurance of emergency medical care practices by providing field supervision and evaluation of emergency care personnel and investigation of incidents.
- Maintain statistics on emergency care incidents and operations as designated by the EMS committee of the medical society and fire board.
- Provide supervision and enforce disciplinary action procedures.
- Supervise the use of biomedical and EMS communications and maintain updated communication procedures.
- Develop and coordinate emergency care training programs for the general public.
- Assist with dissemination of information regarding emergency medical services to public and professional groups.
- Develop and maintain an evaluation of the EMS program and report results to the appropriate agency.
- Assist in disaster planning and training in EMS with the Department of Fire and Rescue Services and other county agencies.
In addition to this, members of the staff also represent the fire and rescue services on local and regional emergency medical services advisory councils.
The Montgomery County Fire and Rescue Services has always had a very close working relationship with the medical society. The EMS committee of the Montgomery County Medical Society is responsible for the medical aspects of fire and rescue services’ prehospital emergency care system.
Medical protocol developed
In 1974, when the MICU program was initiated, the medical society developed a medical protocol for use by fire and rescue personnel. The protocol provides guidelines for routine patient care practices and has a limited number of standing orders which paramedics are allowed to implement while attempting to, or when unable to, communicate with a physician. The medical protocol also contains a physician’s protocol which serves as a guideline to standardize the administration of emergency care without superseding a physician’s prerogative to order treatment according to his own judgment. The medical society’s EMS committee reviews the protocol annually and has increased the number of paramedics’ standing orders for definitive treatments.
The physicians from the medical society also supervise maintenance of the EMS quality assurance program. They were instrumental in the creation of a field supervisor position in the EMS section of the Department of Fire and Rescue Services. Three field supervisors (sergeants in the EMS career ladder) were hired and their main responsibilities include making rounds at all the MICUs to review all incidents for adherence to medical protocol, making rounds at the local hospitals and providing assistance and supervision on complex incidents. When violations of the medical protocol or medical practice are discovered or reported, the field supervisors investigate and gather data for the physicians to review. If disciplinary action is indicated in a situation, the physicians use the paramedic performance standards review procedure developed by the EMS committee of the fire board.
As mentioned previously, medical direction is provided by the physicians in the emergency departments at the four county community hospitals. The EMS staff maintains close liaison with the emergency hospitals so that any problems arising between emergency care personnel in the fire and rescue service and hospital personnel can be resolved as soon as possible. In-service programs on subject matters pertaining to the fire and rescue services operations are conducted yearly at each of the hospitals, and hospital personnel are encouraged to ride ambulances and MICUs as an orientation and educational process.
Uniform standards and policies have been a key factor in the effectiveness of using both career and volunteer personnel in the emergency medical services system in Montgomery County. Having the best of both worlds has facilitated a more rapid expansion and upgrading of the emergency medical services than would have been possible in a totally career or totally volunteer system.

