CULTURED SKIN GRAFTS— A Theoretical Possibility Recomes a Medical Reality
A medical breakthrough in the treatment of burn patients saved the lives of two young boys who were burned on more than 95% of their bodies.
RESEARCH

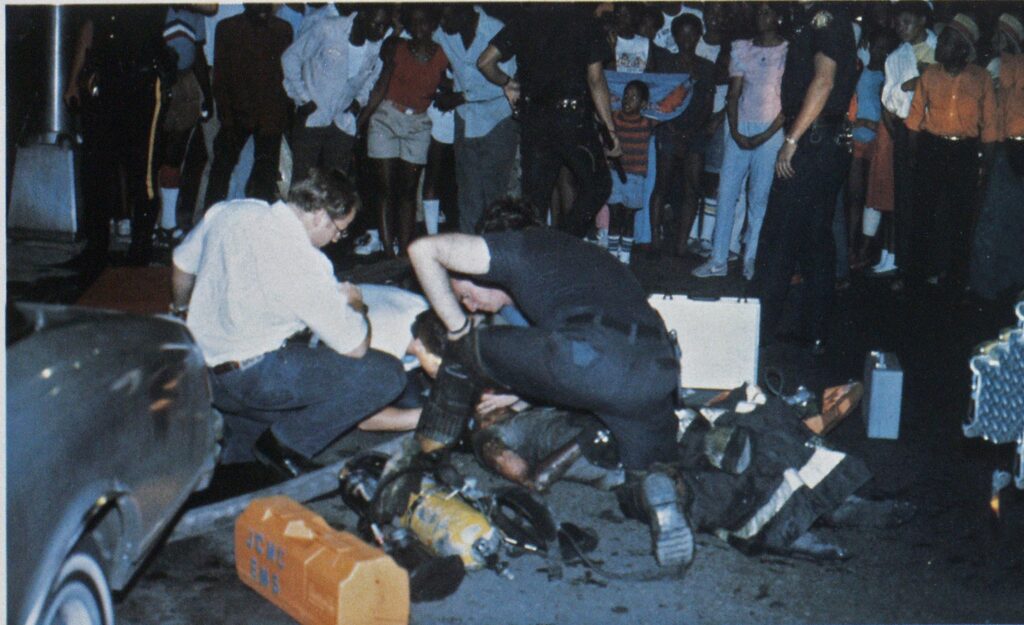
Photo by Ron Jeffers
“The widespread clinical use of … skin grafting is a refinement of the World War II era and stands as the most important advance in burn surgery during this or any previous century” said Jack C. Fisher, M.D., of the University of California at San Diego in the August 16, 1984, issue of THE NEW ENGLAND JOURNAL OF MEDICINE.
Last summer, a medical team at the Shriners Burn Institute, part of Massachusetts General Hospital in Boston, made a further breakthrough in skin grafting when they grew tiny patches of skin taken from two severely burned youngsters into sheets sufficient to cover the entire burn surface. This new technique enabled the doctors to save the lives of the two boys, ages five and six, who suffered secondand third-degree burns over 95% of their bodies. The children accidently came in contact with a flame when they were using a solvent to remove paint from themselves.
According to one member of the burn team, the boys “had practically no other hope for survival.”
Method used to grow skin grafts
Two square centimeters of skin taken from the boys’ armpits were minced and mixed with an enzyme to produce single-cell suspensions. These suspensions were grown in test tubes for 10 days, after which the resulting 75 cm2 sheets of skin were again mixed with an enzyme and inoculated. After another 10 days, these 2 X 3-inch sheets of skin, two to eight cell layers thick, were placed on Vaseline gauze and sutured in place on the burn victims.
After several days, the skin grafts adhered to the tissue and muscle of the wounds. After 14 weeks, the grafts grew into skin tissue of normal thickness, but lacked nerves, sweat glands, and hair follicles. The absence of these specialized structures has not caused any medical problems, according to the burn team. The overall expansion of the skin was 10,000 times its original 2 cm2.
Initial results
The five-year-old boy, Jamie Selby of Casper, WY, who sustained burns on 97% of his body, received 146 cultured skin grafts, which covered 49% of his body. After 21 weeks in the hospital, his wounds were 98% healed.
Jamie was able to return home for two to three months after being hospitalized for eight months, according to Nicholas E. O’Connor, M.D., a member of the burn team.
Jamie’s brother Glen, six years old, sustained burns on 98% of his body, and received 233 cultured skin grafts, which covered 54% of his body. After 23 weeks in the hospital, Glen’s wounds were 85% healed.
According to the burn team, considerably fewer operations were performed on the Selby boys than would normally be required if the new grafting technique had not been used.
At presstime, both boys were scheduled to go home at the end of September and will return to the Shriners Burn Institute a few times a year for reconstruction.
Between 70% and 80% of the cultured skin grafts succeeded in adhering to and growing on the boys’ bodies. Both boys still face a number of years of plastic surgery, physical therapy, and rehabilitation counseling.
The Selby brothers were the ninth and tenth patients to have their burns covered with cultured skin since the technique of growing cultured skin grafts was first developed in 1974 by Howard Green, M.D., at Harvard Medical School in Boston. Green headed up the medical team that grew the skin grafts used in the 10 burn cases. The technique of grafting cultured skin on a burn victim was first used by Dr. O’Connor in 1978.
Problems of skin grafting
The amount of skin that can be grafted at one time is limited by how long a patient can remain under general anesthesia, which is necessary due to the painful process of grafting. The length of time a patient can be anesthesized depends on his general condition.
While the skin grafts were being grown, the Selby boys were kept alive with massive amounts of intravenous fluids and antibiotics. Dead tissue was cut out periodically, and superficial second degree burns were allowed to heal and then used as donor sites for standard skin grafts. The boys were also covered with sheets of collagen (an insoluble fibrous protein) and with skin grafts from human cadavers. Although vital on a temporary basis, these skin grafts are eventually rejected by the burn victim because skin (the body’s largest organ) rejects genetically dissimilar tissue.
Previous work done with cultured skin grafts (on a much smaller scale) has shown that the body accepts the cultured skin, which is durable during normal activities.
Another problem with skin grafts is wound contraction. Any wound, explains Dr. Fisher, large or small, seeks to close itself, and wound contraction leads to deformity, especially across joint surfaces. Fisher adds that “Clinical experience shows that wound contraction can be halted almost completely by the application of fullthickness skin—i.e., by a graft consisting of both epidermis and dermis. Split-skin grafts include the epidermis and only a portion of the dermis; they slow the contraction process but cannot stop it altogether.”
Summary
Extensive burns are among the most painful and difficult to treat of all health problems. “Until immune barriers can be more selectively and effectively interrupted,” says Fisher in THE NEW ENGLAND JOURNAL, “the autologous host (skin grafts from the burn victim himself) remains the best source of the tissue most necessary for burn recovery.”

