By JERRY BIGGART
As a current and future fire service leader, you are responsible for ensuring that your fire department is better positioned to provide emergency medical services (EMS) in your community than other organizations and companies. An estimated 36,698,670 EMS events (responses) occurred in the United States in 2009.1 Many would argue that an all-hazards fire-based EMS provider is the best way to handle a vast majority of these responses. The caveat to the previous statement, however, is that you must ensure that the fire-based EMS service is providing the highest level of care, treatment, and transport that its system’s scope of practice allows.
There are many reasons and excuses for a service or system’s not maximizing its potential. In addition, there are hurdles out of the service’s control such as the state or a medical director who won’t add time critical and beneficial skills to an emergency medical technician’s (EMT’s) scope. So, there are two sets of circumstances in play. First, the EMT has not been given the skill by the state or its medical director or the service has not embraced the full scope of practice allowed by the state in which he practices. In the United States, 12 states (24 percent) maintain a list of procedures at the state level that have been approved for use at each EMS professional level. (1) The remaining states allow the determination of medical procedure use to be determined by the local EMS medical director.
The questions remain: Can you do more for your patients? And, are you treating your patients as if they have a choice? In most metropolitan areas, citizens can call 911 or a seven-digit number for their EMS needs. If you aren’t providing a high level of medical care with the same level of customer service, they may very well call there instead. And, if your response to that statement is, “Good, call someone else,” you have a limited amount of time to embrace EMS from a very different perspective.
In this economic climate, all fire service leaders (not just chiefs) are facing difficult, often unprecedented, decisions. Municipal attempts to close budget gaps are being placed on the backs of the fire service as never before. All of the easy budget cuts have been made and, for the first time in many of our careers, the long-term health of our fire departments is in jeopardy.
In fall 2011, a New York Times poll revealed that 89 percent of Americans distrust government to do the right thing.2 Politicians and municipal managers are under immense pressure to make government more productive and efficient without raising tax dollars. At the end of the day, most of us work for the government, which makes us the government. To some, we have gone from role models to villains because we are fairly compensated for our job.
Throughout the nation, fire departments are being told that they no longer have the right to provide service to its citizens because private companies are moving into their bays. The same politicians who dismantle fire departments have their hand out and take campaign contributions and PAC money from the private companies that are putting us out of business. All you have left are your citizens, and you need to give them as many reasons as possible for not throwing their sick or injured family member into a pickup truck and driving him to the hospital themselves. Ensure that you show the value in what you do and that you are expanding your system. If you don’t, fire-based EMS will become increasingly irrelevant.
Can you get past some of the attitudes? Yes! It’s not the 1970s or 1980s anymore. If there are firefighters on the job hired in the past 20 years who didn’t come on the job to do EMS, they did nothing to prepare for their career. That being said, there is nothing more valuable on the fire scene than a confident, competent fire officer or firefighter, but this article focuses on the other 70-plus percent of what you can provide to your citizens, which is largely fire-based EMS.
Fires and fire-related responses are decreasing, but people are turning 65 at a rate of roughly 7,000 per day.3 Thus, the EMS needs of the Baby Boomers will be remarkable. Fire departments in the business of EMS must embrace all of its aspects and become innovative in ways that expand their service and add value to the community; fire departments that do not should begin exploring every option to get into the business provided they have the will and they can see why it’s important. For some time, there existed the adage, “They can privatize EMS all they want, but they are still going to need a fire department.” I challenge anyone who believes this to look around the United States and Europe before uttering those words again. There are full service companies that can and will do it all.
The National EMS Assessment released in late 2011 by the Federal Interagency Committee on Emergency Medical Services amplified that the largest provider of EMS in the United States is the fire service. (1) Do you want to keep it that way? If your answer is yes, you have a lot of work ahead of you just to maintain your current status. Ensure that you are fully embracing EMS as a mission of the fire service and are not looking at it as a necessary evil. This will require a cultural shift in some organizations. Additionally, some organizations will ignore the warning signs and wait until their only option is a strong defense. If you have doubt about what may be coming to your community, please review the analyses of fire departments such as Grand Rapids, Michigan, that have been conducted by the ICMA Center for Public Safety Management.4
The rest of this article will review EMS system performance standards, many of which have been identified by the International Association of Fire Chiefs (IAFC) and the International Association of Fire Fighters (IAFF). These performance standards allow organizations to measure their EMS system and its capabilities. The data collected in the performance standards are one of the few ways that you can justify what you do and why you do it. An emotional argument over staffing, service, apparatus, station placement, and budgets is no longer a viable option. When a fire service leader tells a city manager that he needs something, that leader must come armed with data and know how to talk to someone who knows far less about the fire service than he does. When a 20- to 30-page report from the fire department gets stuffed in an elected official’s mailbox or is given to a city manager, it is very unlikely that much will be done with it. How you package the data is just as important as the data.
TREATMENT AND PROCEDURES
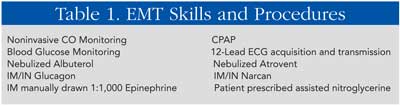
I asked previously if you are doing everything you can for your patients. Let’s look solely at the basic life support (BLS) provider and what it can offer beyond the 2009 National EMS Education Standards. Table 1 is a checklist of skills and procedures that EMTs in varying states have as part of their scope of practice.
Throughout the nation, essentially every EMT-basic can administer epinephrine through an auto injector. However, consider the cost savings of manually drawing up epinephrine and replacing the expired adult and child auto injectors. Consider how cost effective it would be to put epinephrine in all units that may respond on EMS calls. The equipment required for a manually drawn epinephrine injection for anaphylaxis costs roughly $3 and covers all ages. A typical epinephrine auto injector costs roughly 15 to 20 times that, and you need one each for an adult and a child. There is no more money, so you must save it where you can and redirect it to other areas of the program.
PATIENT OUTCOME
For my entire career, EMS has been focused on one main patient care-related question: Did you get the patient’s pulse back?
Why do you spend so much time focusing on roughly one percent of your EMS calls? Because it’s easy to measure and easy to track. You showed up, the victim was without a pulse, and you delivered him to the hospital with a pulse. Then, you receive another gold star if he lived for 24 hours after you got his pulse back! Isn’t the true measure of a responder if the patient left the hospital neurologically intact?
Has your organization established a program with its receiving hospitals to have access to those data? Better yet, what is your organization doing to track information such as how many congestive heart failure and chronic obstructive pulmonary disease victims didn’t need to be intubated because EMS quickly provided the appropriate treatments such as nitroglycerine, continuous positive airway pressure, and so on? Are you tracking your successes of transporting trauma, ST segment elevation myocardial infarction, and cerebral vascular accident patients to the appropriate hospital within the acceptable window of time? You need these data to justify your current EMS system and staffing, its advancement, and your budget. Your data collection should focus on patient outcome just as much as arrival time at the event.
QUALITY IMPROVEMENT, MANAGEMENT, AND ASSURANCE
How does your EMS system measure its quality? Without quality management, it is virtually impossible to monitor compliance and improve a system and identify problems and successes. Many fire-based EMS organizations say that they have quality assurance in place, but often issues are only discovered through the complaint process. It is recommended that the following practices be in place:
Continuous quality improvement. It allows the organization to look at all activities that are undertaken to examine and improve the products and services continuously, including using system performance measures to compare the system to itself over time.
Total quality management. It requires an absolute commitment from top leaders to identify measurable and accurate indicators of quality and to involve stakeholders in all quality improvement efforts.
Quality assurance. It represents the performance measure of structure, process, and outcomes within the EMS system and its comparison against a standard.
PREARRIVAL INSTRUCTIONS
What is your dispatch center providing to the 911 caller? In many areas of the country, dispatchers are answering the call, obtaining the address and nature of the call, and telling the caller that “help is on the way.” Communications centers, at minimum, must begin providing prearrival instructions for incidents that require time-sensitive intervention. To demand prearrival on all incidents isn’t necessary, but it should occur for compression-only cardiopulmonary resuscitation (CPR), complete airway obstruction, and uncontrolled bleeding.
The 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care recommend that bystanders immediately call their local emergency response number anytime they find an unresponsive patient and that all dispatchers be appropriately trained to provide effective CPR prearrival instructions.5 Effective CPR prearrival instruction programs can nearly double the rate at which you perform bystander CPR. Even in communities where the EMS response is exceptionally quick, a structured CPR prearrival instruction program can provide a measurable benefit.6
Implementing new initiatives in communications centers can be difficult because most of them are controlled by the police department. It is simple for a police manager to make a compelling case not to offer prearrival by citing cost, training, and taxing of the personnel. In reality, the training is minimal since dispatchers can read the information word for word; you do not have to use a commercially created, costly program. The events where prearrival instructions are required do not occur as often as other calls for service. A free prearrival instruction plan can be accessed by the link at the end of the article and modified to fit your service and after medical director approval.
NFPA RECOMMENDATIONS
Although not all agree with National Fire Protection Association (NFPA) recommendations and standards, a critical factor in the effectiveness of any emergency response agency is the ability to get personnel and equipment to the scene of the emergency in a timely manner. As stated earlier, the data should also be geared toward patient outcome and the evidence that supports it. NFPA 1221, Standard for the Installation, Maintenance, and Use of Emergency Services Communications Systems, states the following:
- Ninety-five percent of all 911 calls must be answered in 30 seconds.
- Dispatch of emergency response aid shall be made within 60 seconds of the completed receipt of the emergency alarm.
- Ninety-five percent of all calls must be processed in less than 90 seconds.
- The goal is to meet this guideline 90 percent of the time.
It is important to track the reasons for noncompliance. The data may show that language barriers and cultural competency issues need to be further addressed, that the workload is not practical for the communications center staff, that a specific dispatcher requires additional training, and so on. Unfortunately, many organizations never look into the situation unless it caused identifiable problems on scene. Dispatchers tend to know very little about the fire service. It is extremely important that fire leadership be involved in dispatcher training and job performance requirements.
The time from alert to wheels turning provides an indication of the state of readiness of personnel. Minimizing this time is crucial to an immediate response. NFPA 1710, Standard for the Organization and Deployment of Fire Suppression Operations, Emergency Medical Operations, and Special Operations to the Public by Career Fire Departments, states that the turnout time shall be one minute.
Travel time, identified as wheels rolling until on-scene arrival, is indicative of the system’s capability to adequately staff, locate, and deploy response resources. It is also indicative of responding personnel’s knowledge of the area and efficient travel. NFPA 1710 allows for the following:
- An EMS first response in four minutes or less;
- within eight minutes of an advanced life support (ALS) response, an ALS provider on scene 90 percent of the time; and
- an appropriate transport capable vehicle on scene within eight minutes 90 percent of the time.
The NFPA standards should be tracked and help the service identify quantitative data that can be used to help craft arguments for additional staffing or a new station. The level of EMS training of personnel deployed (ALS or BLS) is indicative of the quality of the service delivered and, therefore, the system. Anecdotally, two or more advanced EMS personnel are considered higher quality than one. Although many individual state regulations consider one paramedic as an adequately staffed ALS unit, NFPA 1710 requires two paramedics for compliance as an ALS unit. For compelling arguments to justify the appropriate staffing of personnel on EMS incidents, review the National Institute of Standards and Technology (NIST) report on EMS Field Experiments.
PROTOCOL COMPLIANCE
Compliance with established patient care protocols is intuitively related to the quality of the care delivered in the EMS system. The quality of the care then relates to the overall quality of the system. The data can be collected through comparison of patient care documentation with established written (recognized) patient care protocols.
If there is missing documentation, a protocol violation, a medication error, and so on, explaining the concern to the EMT and offering remedial training will be of much greater value than discipline. It’s extremely rare to find a firefighter who came to work planning to deliver poor patient care. Crisis managers, firefighters, and EMS personnel are bound to make isolated errors. When errors occur, it becomes a leader’s job to embrace the error, figure out why it occurred, and then counsel and instruct the member to minimize the chance that the same error would happen again. When problems are handled fairly and equitably, EMS providers have a much better likelihood of remaining engaged stakeholders in the organization. Save the formal discipline for issues that warrant it. Rarely is it warranted for an accidental error in patient care.
NO TRANSPORTS
Does your organization track no transports? More specifically, do you have a mechanism in place to recognize when there is a second call for service to the same location or when a death occurs at the same location within 24 hours of the first call for EMS? The art of not transporting patients is one of the most important skills of an EMS provider, yet hardly any time is spent teaching an EMT the skill. The curricula that cover medical legal issues are typically minimal and covered in one of the first days of class and very little thereafter. Ensure that the EMS providers review no-transport criteria regularly, especially in the area of patient competency and medical power of attorney.
The performance standards discussed in this article are just some of the standards that services should be measuring. I encourage you to review the 2011 National EMS Assessment Report, the IAFF/IAFC EMS System Performance Measures, and the NIST EMS Deployment Report. The IAFC summarizes fire-based EMS well:
| “Fire service EMS is the most efficient and effective model for the rapid delivery of all emergency medical services. When time is critical and effective pre-hospital care is necessary, the fire service is well positioned strategically, geographically, administratively, financially, and operationally. Therefore, the International Association of Fire Chiefs urges all elected and government appointed officials, professional associations and health care providers to recognize and support the provision of emergency medical care first response and ambulance transport by the fire service.”7 |
The vulnerability of fire-based EMS is here to stay. There is no one more capable of delivering high-quality prehospital medical services to the nation’s population than fire- and government-based EMS systems. Become engaged, ask the tough questions, and dedicate your time to gather the data that will be needed to defend the attacks against our profession. The attacks have only just begun. Prepare your offense now with the limited time you have!
ENDNOTES
1. Federal Interagency Committee on Emergency Medical Services. National EMS Assessment. (2011). Retrieved from http://ems.gov/pdf/2011/National_EMS_Assessment_Final_Draft_12202011.pdf.
2. Zeleny, J and M Thee-Brennan. “New Poll Finds a Deep Distrust of Government.” New York Times. October 25, 2011. Retrieved from: www.nytimes.com/2011/10/26/us/politics/poll-finds-anxiety-on-the-economy-fuels-volatility-in-the-2012-race.html?_r=0.
3. Love, J. Approaching 65: A Survey of Boomers Turning 65 Years Old. December 2010. Retrieved from: www.aarp.org/personal-growth/transitions/info-12-2010/approaching-65.html.
4. ICMA Center for Public Safety Management. Final Report, Fire Operations, Grand Rapids, Michigan. August 2012. Retrieved from http://grcity.us/city-manager/Documents/Grand%20Rapids%20Fire%20Ops%20Final%2014AUG12.pd.
5. Emergency Medical Service Dispatch Cardiopulmonary Resuscitation Pre-arrival Instructions to Improve Survival from Out-of-Hospital Cardiac Arrest. American Heart Association. October 12, 2011. Retrieved from: http://circ.ahajournals.org/content/125/4/648.full.
6. Pirrallo, R. Milwaukee County EMS Guidelines and Pre-Arrival Instructions. December 12, 2010. Retrieved from http://county.milwaukee.gov/ImageLibrary/User/jspitzer/EMSDispatchGuidelines/3TieredPrearrivalLightsandSiren030510.pdf.
7. International Association of Fire Fighters and International Association of Fire Chiefs. EMS System Performance Measurement Operations Manual. Retrieved from: www.iaff.org/tech/PDF/EMSSystemPerformanceMeasurement.pdf.
● JERRY BIGGART is an 18-year fire service veteran and a career lieutenant/paramedic with the City of Oak Creek, Wisconsin. He is an EMS instructor/coordinator for the Milwaukee (WI) Fire Department, a fire/EMS instructor at several technical colleges in southeastern Wisconsin, and a member of the Wisconsin EMS Advisory Board and chair of the EMS Education & Training Committee.
Fire Engineering Archives

