At 2251 hours on December 1, 2015, the tones went off at Fire Station 3 in midtown Reno, Nevada. The dispatch called for Battalion 2, Rescue 1, Engine 3 (E3), Engine 5, Engine 21, Truck 3 (T3), and Training 1 to a structure fire with flames seen.
E3, usually a newer pumper but a reserve 1987 rig that evening, pulled out of Station 3 followed by T3 (a tillered 100-foot aerial ladder truck) and the battalion chief (BC) in his SUV. This was another run of the station’s average of 17 runs every 24 hours.
The truck captain located the preplan for the structure, a two-story wood-frame apartment complex. Dispatch delivered an update that advised of heavy smoke and the possibility of an occupant trapped on the second floor.
On Scene
E3 arrived on scene and delivered a size-up. The BC assumed command, and E3 took the attack group. T3 was assigned rescue and ventilation.
Thick black smoke billowed from a second-story window on the C side of the apartment complex, opposite a breezeway with two units on the ground floor and two stairways to the second-story units.
The truck captain ordered an extension ladder to the C side for rescue and topside ventilation. The truck carried 16- and 20-foot straight ladders in its complement, both of which could be carried by a single firefighter, but the captain wanted something that would work for both a rescue and for getting to the roof of the complex. The mudflap (the junior firefighter on the truck who sits behind the captain) also had the option of a 24-foot extension ladder for a single-person throw, but it was not part of the truck’s ladder complement, only the engine’s. At that time, the side board of the pumper was busy with hose being pulled and the operator spinning off a blind cap (the crosslay on the older rig was not a preconnect).
The mudflap hopped out of the tractor and selected the 28-foot extension ladder to slide out from the rear of the truck as the tillerman strapped on his self-contained breathing apparatus (SCBA). The tillerman took the butt end of the ladder, and they did a low-shoulder carry past the engine company that was stretching a shoulder load of 1¾-inch attack line to the second story.
The Rescue
Around back, a woman was straddling the open sill of a double-sliding, second-story window, leaning under the heavy smoke, looking as if she wanted to jump. The engine captain held out a staying hand and told her to hold tight, help was coming, and to hang on just another minute. Upstairs, one of the engine firefighters burro-kicked open the locked front door only to find that a living room couch had been placed in front of it.
The mudflap and tillerman did a beam-raise of the 28-foot ladder and placed it as optimally for rescue as possible, given that a large tree inhibited their access to the second-floor window. (They reported in retrospect that a flat raise would have been mechanically easier.) The mudflap also reported later that he had tightened his SCBA shoulder straps too tight and tended to knock the rear brim of his helmet on the top of his bottle when he looked up. The 28-foot ladder was long, still measuring about 16 feet with the fly bedded, which made the ladder tip almost even with the top of the window frame instead of at the sill, the ideal placement. Additionally, a large evergreen tree would not allow the firefighters to place along the wall just adjacent to the window opening the woman was straddling. They had to set up the ladder a few feet away alongside the wall of the closed window.
One firefighter ascended the ladder while his partner footed it from behind with both hands; the ladder’s butt end was driven into the dirt. When the firefighter reached the window, he kept one hand and one foot hooked along the window-side ladder rail and stretched his other leg out to the wall just below the open window the woman was straddling. He reached out with his arm. In one motion, the woman clutched his neck and set her weight on his thigh. He drew her back to the ladder, cradling her torso by holding the rails, and lowered her on his leg rung by rung. They made it to the ground. He carried her to the front where he had her sit on the concrete steps. Her face was thoroughly soot stained, and she had the look of a woman anxiously searching for something off in the distance.
Patient Medical Evaluation
The truck operator brought the medical first-out bag and confirmed that the private ambulance company was not yet on scene. He took baseline vitals: diastolic blood pressure was slightly elevated, respirations 24 with moderate effort, oxygen (O2) saturation 89 percent on ambient air [though unreliable because of the likelihood of carbon monoxide (CO) inhalation, yet still a concern given the low reading], radial pulse was strong and regular at 140 beats per minute-sinus tach on the monitor with no ectopy. He set up a nonrebreather O2 mask at 15 liters per minute. The mudflap attempted to ask the basic A and O questions. All the patient wanted to talk about was her cat.
One of the engine firefighters showed up with a frazzled and mucked up orange feline-arms and legs outstretched and claws spread, a glazed dysconjugate gaze in its eyes-the patient looked relieved and took it underarm, its legs dangling and paws still straightened.
The engine captain reported knockdown of the fire, and the truck operator attached a CO pulse oximeter to the patient, eventually getting a carboxyhemoglobin reading of 10 percent-the lowest value needed to put the monitor into an alarm state. A quick listen to lung sounds in the posterior bases revealed fine rales.
The firefighters tried to explain to the patient the need for transport, that she inhaled a lot of toxic smoke and that her lungs were reacting to it in a way that would probably get worse. She was anxious and did not like the idea of the ambulance or the hospital. Although she was able to answer correctly to person, place, time, and event, she had an underlying agitation about her. Pupils were normal, and no odor of ETOH (ethanol) was noted.
The ambulance arrived, and the firefighters were able to convince the patient to get into the back for further evaluation. She was apprehensive, but she agreed; care was transferred to the transport paramedics.
On scene, crews were only part way through overhaul of the fire when they received the report that the patient had thrown open the back doors of the ambulance and leaped out, cat still in arm, and ran barefoot down the street away from the scene.
Post-Incident EMS Evaluation
The patient was not altered by basic definition, but she was not acting “normal” either. The fire inspector listed the cause of the fire as accidental and secondary to unattended smoking materials on a couch. Reportedly, the patient had a habit of placing her couch across the front door at night for security reasons. It did not appear from the investigation that the patient had anything to hide. So the question remains, why was she so agitated?
She did register an SpCO® of 10 percent on the pulse CO-oximeter, the lower end of CO poisoning but perhaps enough to show minor symptoms. However, with marked smoke inhalation, as the situation evidenced and the soot staining around her airway indicated, she also could have been suffering from a mild form of cyanide poisoning.
Cyanide has been detected in fire smoke and in the blood of fire victims, giving rise to a theory that cyanide poisoning may play a significant role in smoke inhalation.1-2 With the availability of a safer cyanide antidote kit in the United States (hydroxocobalamin), many emergency medical services (EMS) protocols include cyanide antidote treatment to victims of smoke inhalation who are in respiratory or cardiac arrest or have profound hypotension with altered mental status.
Tachycardia is a known early symptom of cyanide poisoning, followed by a stuporous or combative phase.3 Perhaps a more detailed evaluation of the patient’s mentation-quantifying her verbal responses according to the Glasgow Coma Scale (GCS)-might have eventually produced a “confused” or “inappropriate” response with a GCS of 13 or 14 (out of 15 total).
What can you do if a patient is “technically” alert and oriented but unwilling to agree to transport despite signs, symptoms, and a situation (in this case, smoke inhalation) that may impair the ability to exercise sound medical judgment? One answer may be to allow the patient to talk long enough to ascertain and legally establish that he is or is not altered by medical legal definition.
Field protocols for a cyanide antidote kit often only address unconscious, unresponsive patients pulled from a structure fire. Should conscious smoke inhalation patients be tested for cyanide in the field? Unfortunately, there is no single rapid blood test for cyanide; even if one were available, interpretation would be difficult because cyanide is a normal metabolite in humans. Cyanide blood testing done in hospitals is typically sent to one of only a half dozen approved labs, and results take several weeks to report.
However, elevated blood lactate levels have been suggested to lend diagnostic weight to suspected cyanide poisoning. A lactate greater than 10 millimoles per liter in a smoke inhalation patient is often used as an indicator of considerable cyanide exposure.4 Lactate levels can be measured in the field through point-of-care (POC) blood testing devices. Studies comparing finger stick POC lactate levels with traditional hospital lab results found good correlation.5 Since those studies were conducted, the U.S. Food and Drug Administration has approved other POC lactate devices that range in price from relatively inexpensive (several hundred dollars) to very expensive ($6,000 to $10,000).
So what is the takeaway? Perhaps our EMS systems should consider a field protocol for the administration of a cyanide antidote kit for the smoke inhalation patient who is conscious, anxious/agitated, tachycardic, and tachypneic and who has elevated lactate levels.
Reportedly, the morning after the fire, a friend of the patient found her wandering the apartment complex in moderate to severe respiratory distress. The patient finally agreed to go to the emergency department with her friend. Cyanide references suggest that a patient with acute poisoning from cyanogens may not show signs or life-threatening complications for many hours after exposure.
Do cyanide antidote protocols need to be expanded? Are we inadequately protecting patients whose judgment and reasoning may be biochemically impaired? As fire crews, we put so much on the line to exact an effective rescue; how can we best ensure that our efforts are not in vain?
Follow-Up
As a result of the insights garnered through this fire rescue call, the Reno Fire Department has drafted an advanced life support smoke inhalation protocol that includes the authorization to administer a cyanide antidote kit not only to patients in cardiac arrest or with profound Adult Level of Care and hypotension but also to those exhibiting signs and symptoms consistent with cyanide toxicity. Additionally, our department recently received a federal grant for the purchase of hydroxocobalamin cyanide antidote kits.
References
1. Barillo DJ, Goode R, Esch V. “Cyanide poisoning in victims of fire: analysis of 364 cases and review of the literature,” J Burn Care Rehabil 1994;15:46-57.
2. Anderson RA, Harland WA. “Fire deaths in the Glasgow area: III the role of hydrogen cyanide,” Med Sci Law 1982;22:35-40.
3. Gossel TA, Bricker JD. “Characteristics of Poisoning,” Principles of Clinical Toxicology. New York: Raven, 1994. 116. Print.
4. Baud FJ, Barriot P, Toffis V, Riou B, Vicaut E, Lecarpentier Y, et al. “Elevated blood cyanide concentrations in victims of smoke inhalation,” N Engl J Med. 1991; 325:1761-1766.
5. Gaieski DF, Drumheller BC, Goyal M, Fuchs BD, Shofer FS, Zogby K. “Accuracy of handheld Point-of-Care fingertip lactate measurement in the emergency department,” Western Journal of Emergency Medicine. 2013;14:58-62.
Shawn Grady is a firefighter/paramedic with the Reno (NV) Fire Department and a per-diem EMS instructor at Truckee Meadows Community College. He is the author of three emergency suspense novels-Through the Fire, Tomorrow We Die, and Falls Like Lightning.
RFD: Smoke Inhalation/Cyanide Poisoning
Issued: 5/1/2016 PARAMEDIC Revised: Scene safety and BSI
ASSESSMENT
TREATMENT
 |
|
Figure 1. Reno (NV) Fire Department Smoke Inhalation/Cyanide Poisoning Protocol for Paramedics (issued May 1, 2016) |
Complete Starting Dose: 5g
-
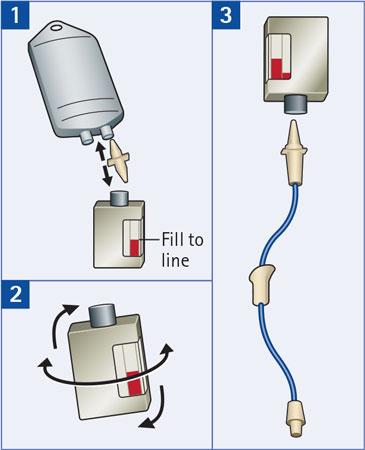
Reconstitute: Place the vial in an upright position. Add 200 ml of 0.9% Sodium Chloride injection* to the vial using the transfer spike.
Fill to the line.
*0.9% Sodium Chloride injection is the recommended diluent (diluent not included in the kit). Lactated Ringer’s injection and 5% Dextrose injection have also been found to be compatible with hydroxocobalamin and may be used if 0.9% Sodium Chloride is not readily available.
-
Mix: The vial should be repeatedly inverted or rocked, not shaken, for at least 60 seconds prior to infusion.
• CYANOKIT solutions should be visually inspected for particulate matter and color prior to administration.- Discard solution if particulate matter is present or solution is not dark red.
- Discard solution if particulate matter is present or solution is not dark red.
- Infuse Vial: Use vented intravenous tubing. Hang and infuse over 15 minutes.
PATIENT HISTORY
DIFFERENTIAL DIAGNOSIS
CONSIDERATIONS
CYANIDE POISONING: HOW MUCH 0F A THREAT?
Hydrogen Cyanide : New Concerns for Firefighting and Medical Tactics
Cyanide : Fire Smoke’s Other “Toxic Twin”
Fire Engineering Archives

