
By CRAIG A. HAIGH, DENISE L. SMITH, and ANDREA F. WILKINSON
Firefighters like processes that give step-by-step algorithms to follow. Whether engaging an apparatus pump, setting up the truck for aerial operations, donning self-contained breathing apparatus (SCBA), or mixing a medication and titrating the dosage, we operate best when we have a step-by-step procedure to follow. These steps, when practiced repeatedly, create muscle memory, which allows us to perform a procedure without focusing on the individual aspects of the process. Actually, the term “muscle memory” is not entirely accurate in that your muscles do not remember the steps but rather your brain connects the specific dots needed to perform a skill through repeated practice. Composer and pianist Malcolm Kogut writes, “Practice is not measured in minutes or hours, but in the number of high-quality repetitions you make—basically, how many new connections you form in your brain.”1
Firefighter health is at the forefront of many discussions and much ongoing scientific research. Preventing injuries and illnesses in our first responder population has become a paramount issue in today’s fire service. The significance of this prevention extends beyond the reduction of pain and suffering: It includes the impact to first responder families as well as the costs to the department associated with workers’ compensation claims; disability pensions; shift backfill; and, in the volunteer fire service, the loss or availability of a responder.
By using a step-by-step algorithm, we can break down the complexities of reducing firefighter risks of injury and death and improving fireground performance. Much like the step processes outlined by the Centers for Disease Control and Prevention to mitigate a variety of health concerns, the fire service can follow the same format to teach members steps for decreasing the risks or threats to firefighter health.
Steps for Reducing Health Risks
The following three-step process has been the model taught to emergency responders for many years. The steps outline the basic premise of emergency operations.2 Think of the steps in the same manner as you would if you were handling an emergency response.
- Prepare to respond. Most of us agree that the success of our mission depends on our commitment to the tasks involved in this step: checking our apparatus and tools, ensuring that our personal protective equipment (PPE) is ready to be donned quickly and—if we are coming from home as a volunteer/paid-on-call provider—that our vehicle is fueled and posited for a quick response.
- Use our skills, tools, and equipment to mitigate the incident. After the incident is stabilized, we return to the fire station.
-
Reset our apparatus and tools in preparation for the next emergency response. Once the incident is stabilized, we return to quarters where we reset our apparatus and tools in preparation for the next emergency response.
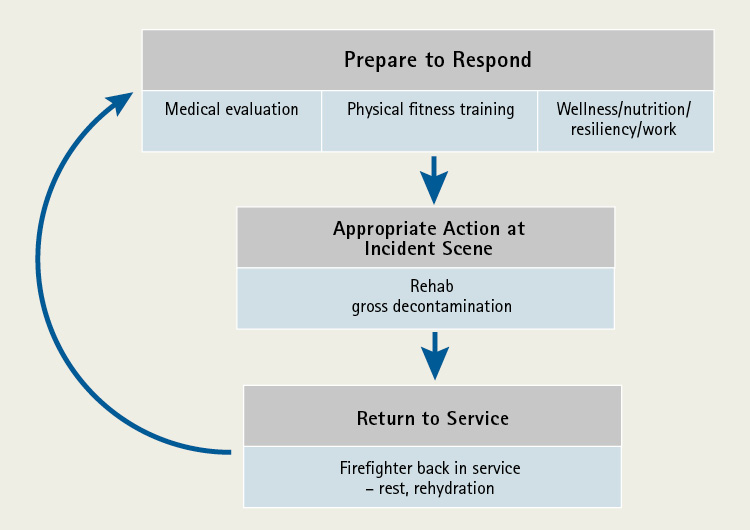
Figure 1. Three-Step Model for Improving Firefighter Health and Safety
Step 1: Preincident
First, ensure that your personnel are physically and mentally fit for duty and able to perform the essential functions of the job. “Being physically fit for duty is one of the most vital and fundamental ingredients of being a successful firefighter.”3
Fitness for duty is a broad category that includes not just how much time you spend in the gym but also your overall health status related to medical evaluations and mental health. Many will argue that health status and fitness are personal issues and have nothing to do with the workplace, regardless of whether you are a career or a volunteer member. This statement, however, could not be further from the truth. Your physical condition has a direct impact on the members of your crew and the public you serve.4
Consider the military. Members are required to develop and maintain physical fitness to ensure that they can meet the physically demanding requirements of their critical work. Likewise, professional athletes are required to maintain a level of fitness and health to perform the demands of their sport.
As firefighters, our battleground, or sporting event, is emergency services, and our game day occurs at the emergency scene. It is essential that we are ready for the demands of the job when the tones drop and we climb aboard the rig and respond to the incident. Anything less than being totally prepared physically and mentally is breaking the sacred vow we have with those who trust us for help in their time of greatest need.
We must see ourselves as occupational athletes who need to maintain our physical conditioning throughout our career. Flexibility, cardiovascular training, muscle development for body areas impacted by job tasks, and good nutrition all work together to maintain functional fitness.5 Simply put, you cannot safely perform the strenuous work of firefighting if you are not physically fit enough to do so.
We also need to stay on top of our overall health through regular medical evaluations using National Fire Protection Association (NFPA) 1582, Standard on Comprehensive Occupational Medical Program for Fire Departments, as the base standard. This industry medical standard provides for the screening and detection of disease, including cardiovascular disease and cancer, to ensure that firefighters are properly treated at an early stage.
The fire service has long known that the leading cause of acute line-of-duty deaths is cardiac events. Research has shown that firefighters have high rates of hypertension, high cholesterol, and obesity.6-8 Regular medical examinations can help to uncover conditions that can be treated, thereby reducing line-of-duty firefighter illnesses and deaths.9
Furthermore, current Federal Emergency Management Agency Assistance to Firefighter Grants-funded research has shown that the vast majority of firefighters who died of cardiac-related events had autopsy-verified atherosclerosis and an enlarged heart.10-11 This indicates that screening to detect disease progression is of paramount importance.
Aerobic fitness (also called cardiovascular fitness or maximal oxygen consumption) is an important part of a medical evaluation. Aerobic capacity is an integrated measure of the ability of the cardiopulmonary system to take in and deliver oxygen to the body and is an important predictor of cardiovascular mortality and morbidity.12 Research indicates, and NFPA 1582 recommends, that firefighters meet at least a 12 MET (metabolic equivalent) level of aerobic fitness.13
Step 2: During the Incident
Firefighters perform strenuous muscular work while wearing heavy protective gear and operate in hot environments. This work leads to dehydration, cardiovascular strain, and thermal strain. Scientific evidence suggests that on-scene firefighter rehabilitation can positively impact these issues and lessen the potential for injuries and death.14
On-scene rehab can be broken into company level rehab and formalized rehab. During company level rehab, firefighters rest, rehydrate, and monitor each other for adverse signs of heat stress or other physiologic concerns. This type of rehab is normally used for situations where firefighters have worked hard and have a basic level of physiologic stress but not to the level classically associated with structural fire attack or similar activities. In these instances, firefighters rehab using bottled water and food products carried on their apparatus.15
Formalized rehab, or “time in the chair” as many firefighters call it, is designed to be a more focused and aggressive process. It includes relief from the climatic conditions, rest and recovery, cooling/rewarming, rehydration, calorie and electrolyte replacement, medical monitoring (including carbon monoxide monitoring, if possible), and member accountability.16
Regardless of whether you are implementing company level rehab or formalized rehab, you have to add gross decontamination and cleaning to the list. During research studies, chemical analysis of firefighters’ hands, neck, and face has shown high levels of total polycyclic aromatic hydrocarbons (PAHs) and benzene. These products were also noted in blood samples taken from firefighters, despite the use of SCBA, suggesting a level of dermal absorption. Using cleaning wipes following firefighting produced a 54 percent reduction in PAH levels on the areas washed.17 Many of these particulates are recognized as carcinogens, and studies have shown a link between the triggering of a cardiovascular event and particulate exposure. (17) Use baby wipes or a similar type product to decontaminate primary areas of exposure to reduce risk.
Likewise, you should grossly decontaminate your PPE while on scene. This is a fairly easy process: Use a shower wand or pressurized sprayer to wet the gear, quickly scrub with dish detergent and a brush, and then rinse. This process has shown to decrease contamination by 85 percent. (17) Apply this same process to your SCBA before stowing it back in the apparatus cab.
It is also recommended that you doff your PPE after decontamination and store it in an outside compartment prior to returning to quarters. This action also reduces cross-contamination with the apparatus cab. (17) As a general rule, though, this entails remembering to toss your shoes into the rig before you leave quarters after donning your gear for the response.
Step 3: After the Incident
Every firefighter knows that it is essential to make sure the apparatus is put back in service after a call. The hose must be reloaded, supplies replenished, and so on. But, what about the most important assets, firefighters? We need to be just as careful in ensuring that we put the “firefighter back in service” in an appropriate way.
Once back in quarters, continued rehydration and caloric intake are musts. Focus on replenishing the fluids lost and replacing calories with foods high in carbohydrates and proteins and low in fats. (14) After especially exhausting fire calls, it may be wise for chiefs to consider leaving companies “out of service” for a time to permit them to recover.
Firefighters need to shower and dress in clean uniforms. The memory inducer taught to firefighters to help them remember this critical risk-reduction step is, “Shower within the hour.”
Volunteer/paid-on-call firefighters are encouraged to keep a change of clothes at the fire station and to shower following the fire response. If your fire station does not have shower facilities, at least wash your face, neck, and hands, and change into fresh clothing before jumping into your car and heading home. This simple act will reduce the risk not only to you but to your family as well.
Finally, cleaning your PPE is essential. The “salty” look of well-used helmets, coats, and pants should not be viewed as a badge of honor but rather as an exposure risk to the firefighters and their coworkers. Launder protective hoods and gloves after each fire. It is also wise to launder coats and pants regularly and to work toward having a second set of gear available for members to switch into after a fire while the other set is being washed.
Firefighter PPE is expensive, and some small departments are challenged to maintain even a single set of PPE for each member. In this case, they should strive to fund two hoods and two pairs of gloves for each firefighter. This will allow the members to replace and launder at least the parts of their PPE that research has identified as the primary sites of greatest exposure to contaminants.
Reducing firefighter risks is a multifaceted and sometimes complex process. The overwhelming amount of information to digest and the corrective actions these data necessitate often can subject firefighters and command officers to “analysis paralysis.” The steps presented here focus on the most important highlights of the current research and offer sound actions that can help reduce firefighter risk in what is becoming a more and more challenging fire service environment.
References
1. Kogut, M. (2017, October 28). How does muscle memory work? Quora. https://doi.org/https://www.quora.com/How-does-muscle-memory-work-1.
2. Grant, H. (1975). Vehicle Rescue. Bowie, Maryland: Robert J. Brady, Prentice-Hall Company.
3. Kerrigan, D, & Moss, J. (2016). Firefighter Functional Fitness: The Essential Guide to Optimal Firefighter Performance and Longevity. Firefighter Toolbox.
4. Jahnke, SA. (2016). Forward. In Firefighter Functional Fitness (pp. 25-27).: Firefighter Toolbox.
5. Jahnke, SA. (2015 December). State of the Science: How Health Behaviors Contribute to LODDs. In DL Smith & K Roche (Chair), Heart to Heart: Strategizing an evidence-based approach to reducing cardiac disease and death in the fire service. Symposium conducted at the National Fallen Firefighters Foundation, Washington, DC.
6. Storer, TW, Dolezal, BA, Abrazado, ML, Smith, DL, Batalim, MA, Tseng, CH, & Cooper, CB. (2014). Firefighter health and fitness assessment: a call to action [Professional Journal Article]. Journal of Strength and Conditioning Research, 28(3), 661-671.
7. Fahs, CA, Smith, D., Horn, GP, Agiovlasitis, S, Rossow, LM, Echols, G, … Fernhall, B. (2009). Impact of excess body weight on arterial structure, function, and blood pressure in firefighters [Medical Journal]. American Journal of Cardiology, 15(10), 1441-1445.
8. Poston, WS, Haddock, CK, Jahnke, SA, Jitnarin, N, Tuley, BC, & Kales, SN. (2011). The prevalence of overweight, obesity, and substandard fitness in a population-based firefighter cohort. Journal of Occupational Environmental Medicine, 53, 266-273.
9. Kales, SN & Smith, DL (2014). Sudden cardiac death in the fire service (Editorial) [Professional Medical Journal]. Occupational Medicine (London), 64(4), 228-232.
10. Geibe, JR, Holder, J, Peeples, L, Kinney, AM, Burress, JW, & Kales, SN. (2008). Predictors of on-duty coronary events in male firefighters in the United States [Medical Journal]. American Journal of Cardiology, 101(5), 585-589.
11. Smith, D. L., Haller, J. M., Korre, M., Fehling, P., Sampani, K., Grossi, K., … Kales, S. N. (2018). Firefighter heart enlargement [Medical Journal]. Journal of American Heart Association.
12. Plowman, SA, & Smith, DL. (2017). Exercise Physiology: For Health, Fitness and Performance (5 ed.). Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins.
13. National Fire Protection Association. (2018). Standard on Comprehensive Occupational Medical Program for Fire Departments [Professional Consensus Standard]. Quincy, MA: NFPA.
14. Smith, DL & Haigh, CA. (2006 April). Implementing effective on-scene rehabilitation [Magazine]. Fire Engineering, 175-187.
15. Haigh, CA. (2018). Firefighter Rehabilitation & Heat Stress Management [Lecture notes]. Retrieved from University of Illinois – Fire Service Institute.
16. McEvoy, M. (2007, December 10). Making Rehab a Requirement: NFPA 1584 [On-line article]. Fire Rescue 1. https://doi.org/https://www.firerescue1.com/fire-rehab/articles/327047-making-rehab-a-requirement-nfpa-1584/National Fire Protection Association. (2014). Standard on the rehabilitation process for members during emergency operations and training exercises [NFPA 1584]. Quincy, MA: National Fire Protection Association.
17. Fent, KW, Alexander, B, Roberts, J, Robertson, S, Toennis, C, & Sammons, D. (2017). Contamination of firefighter personal protective equipment and skin and the effectiveness of decontamination procedures. Retrieved from ULfirefightersafety.org: https://ulfirefightersafety.org/assets/FentEtAl_JOEH2017-0c4af395c0c9165ba4efa971efd01774dd8d6fd35329956184d67eb15c27624d.pdf.
CRAIG A. HAIGH, a 35-year veteran of the fire service, is chief of the Hanover Park (IL) Fire Department and a field staff instructor with the University of Illinois Fire Service Institute. He is a frequent partner with the University of Illinois Fire Service Institute’s Firefighter Life Safety Research Center and the Skidmore College First Responder Health and Safety Laboratory. He is a published author and a national speaker. He has a BS degree in fire and safety engineering and an MS degree in executive fire service leadership. He is a graduate of the National Fire Academy’s Executive Fire Officer Program, is a nationally certified paramedic and an accredited Chief Fire Officer, and is a member of the Institute of Fire Engineers. He was named the 2012 Illinois Career Fire Chief of the Year.
DENISE L. SMITH is professor of health and human physiological sciences at Skidmore College in Saratoga Springs, New York, and a research scientist at the University of Illinois Fire Service Institute. She is director of the Skidmore College-First Responder Health and Safety Laboratory. Her research focus is the physiological effects of firefighting, particularly the cardiovascular strain associated with the combination of heavy physical work and heat stress firefighters routinely encounter. She is the author of Exercise Physiology: For Health Fitness and Performance, which is in its third edition, and of more than 70 scientific peer-reviewed articles. She received the Dr. John Granito Award for Excellence in Fire Service Leadership and Management Research. She earned her Ph.D. in kinesiology with a specialization in exercise physiology from the University of Illinois at Urbana-Champaign. She presents her research and its applications internationally.
ANDREA F. WILKINSON is the project manager for the Skidmore College-First Responder Health & Safety Laboratory. Previously, she spent nine years at Alfred University as the head athletic trainer and clinical coordinator for sports medicine. She attended the University of Akron, where she earned dual bachelor of science degrees in sports medicine for athletic training and exercise science as well as a master of science degree in exercise physiology with a concentration in cardiac rehabilitation. In 2008, she was named an honorary member of Outstanding Women in Education and is an alumna of Leadership Lorain County. She has extensive experience in sports medicine and cardiac rehabilitation through her work with St. Peter’s Health Partners in the CVICU. She has a special interest in preventive medicine for the tactical athlete and first responder.

