By Craig A. Haigh and Denise L. Smith
Even in good economic times, fire departments struggle to find a balance between the desire to implement new and needed programs, including incident rehabilitation, and the reality of finding the resources to do so. The current era of constrained resources makes it even more difficult and stressful for fire department leaders to deliver necessary programs. This article describes how an incident scene rehabilitation (rehab) program can increase firefighter safety and improve on-scene performance, as well as techniques to help leaders identify ways to implement an effective rehab program without negatively impacting overall operational costs.
Incident scene rehabilitation is an intervention to mitigate the physical, physiological, and emotional stress of firefighting; improve performance; and decrease the likelihood of injury or death. Firefighters routinely encounter fatigue, heat stress, and dehydration on the fireground. These stressors impair performance and may present serious health challenges. Firefighting also causes significant cardiovascular strain and, less frequently but even more seriously, can trigger a sudden cardiac event in individuals with underlying cardiovascular disease.
Physical and Physiological Stress of Firefighting
Sudden cardiac events are the leading cause of line-of-duty deaths (LODDs), accounting for approximately 40 to 50 percent of all deaths every year.1 Although firefighters spend a small percentage of their duty time engaged in fire suppression activities, a disproportionate number of sudden cardiac events occur during or shortly after fire suppression activities.2 These data clearly suggest that there is something about the combination of stressors associated with firefighting that can “trigger” a cardiac event.3
The physical and physiological strain of firefighting is caused by a combination of factors. Figure 1 summarizes several of the factors that affect the magnitude of the physiological response to firefighting. Listed at the top of the figure are factors that are external to the firefighter (namely, the work performed, the protective clothing worn, and the environment encountered). Structural firefighting activity encompasses a wide range of work activities, including climbing stairs (or ladders) with heavy loads, interior attack and suppression activities, ventilation operations, and so on. The personal protective equipment (PPE) worn by firefighters is heavy, restrictive, and fully encapsulating, thus adding to thermal and cardiovascular strain. The environment in which the firefighter works varies greatly with different incidents and different jobs on the scene. During structural firefighting activities, firefighters may be subjected to extreme environmental conditions, including temperatures that are not survivable for more than a few seconds. Firefighters are also exposed to smoke and products of combustion on the fireground and often operate in an emotionally stressful environment that elicits a strong sympathetic nervous system response.
As shown in the lower portion of Figure 1, individual factors, including personal characteristics (such as body composition, diet, and genetics); medical conditions (including medications); fitness status; and hydration status also affect the magnitude of the physiological strain of firefighting.
Physiological Responses to Firefighting
Firefighting is strenuous work that results in changes in most all bodily functions.5-8 The physiological changes that are of the greatest concern in terms of the ability to effectively and safely perform firefighting duties are the interrelated issues of fatigue, dehydration, heat stress, and cardiovascular strain.
Firefighters sweat profusely as a result of performing strenuous work in heavy, protective gear, and sweating is exaggerated during structural firefighting, thus increasing the risk for dehydration. Further complicating this issue is evidence that indicates that a large percentage of firefighters are dehydrated before they begin firefighting activity.9-11 Dehydration can cause the early onset of fatigue, interfere with thermoregulation, impair cognitive function, and add to cardiovascular strain. Heat stress is evident in almost all firefighting activity. However, excessive heat stress can be dangerous because of increased levels of dehydration, a breakdown of the thermoregulatory system (heat stroke), and increased cardiovascular strain. All firefighting leads to increased cardiovascular strain, which may limit work performance, but the greatest concern is the possibility of a sudden cardiac event. Firefighting leads to a decrease in plasma volume (5), an increase in heart rate, and increased clotting potential (8); evidence suggests this may increase myocardial dysfunction.12 These physiological responses to firefighting may lead to a sudden cardiac event in susceptible individuals by causing plaque to rupture and a thrombus to form (causing a myocardial infarction) or by causing myocardial ischemia that leads to a dysrhythmia.13 Physiological recovery from firefighting activities can take two or more hours, which further highlights the necessity of on-scene incident rehab.14
Goals and Purpose of Incident Rehabilitation
The primary goal of rehabilitation is to ensure that the physical and mental conditions of members operating at the scene of an emergency or a training exercise do not deteriorate to a point that affects the safety of each member or jeopardizes the safety and integrity of the operation [National Fire Protection Association (NFPA) 1584, Standard on the Rehabilitation Process for Members During Emergency Operations and Training Exercises]. The NFPA standard identifies five specific purposes of incident rehabilitation:
- Provide medical monitoring and treatment if needed.
- Establish standards for food and fluid replacement.
- Provide relief from climatic conditions.
- Provide for rest and recovery.
- Provide for member accountability.
As shown in Figure 2, the components of rehab directly address physiological responses to firefighting.
When fireground rehab was first introduced, there was some resistance within the fire service to embrace the concept. However, fire departments are becoming increasingly more familiar with the benefits of rehab and the impact it has on the safety of their personnel, and they are much more likely to view rehabilitation positively. But, the adoption of rehabilitation policies is still hampered by a lack of resources to implement the program-especially in this time of severely constrained resources.
Leadership Challenge
The fire service is in a challenging position. The downturn in the economy coupled with the public’s demand for increased services has placed departments in a precarious situation. Fire service call volume has increased by 34 percent over the past 33 years. Medical aid responses are responsible for a large portion of this increase. Emergency medical services (EMS)-related responses are up 236 percent (16,327,000 more medical calls). Notable, however, is the fact that overall fire responses are down by more than 1.7 million calls.15
 |
| (1) Medical monitoring must be an integral part of a rehab program and should address the following: mental status, heart rate, skin condition, blood pressure, and respirations. (Photos 1 and 2 by Kenneth D. Zaccard.) |
Yet, even with these significant changes in call volume, the economy has forced departments of all sizes to reduce staffing numbers, resulting in closed companies, rolling brownouts, and fewer firefighters assigned to remaining apparatus. Many departments have suffered huge cuts to staff and middle management positions, resulting in leaders who are exhausted and left challenged to find new options to meet the needs of the communities they protect. Often, we turn to our neighbors for help, which has driven an increase in overall mutual-aid responses of 211 percent (>1,024,000 since 1980). (15) Although it can be argued that this shared use of resources has helped overall operational efficiencies, it can also be said that it has increased the call/workload for assisting agencies and also the cost to some jurisdictions when the “mutual aid” actually becomes a “subsidy” to severely under-resourced neighboring communities/departments.
Impact of the Changing Fire Dynamics
The decrease in staffing becomes even more significant when we consider the fuel load in modern fires. Historically, natural products of wood, cotton, and paper were used to construct the interior finishes and furnishings, which produced around 8,000 British thermal units (Btus) per pound. New construction designs that use plastics, polymers, and laminates have more than doubled the Btu production.16
It is well accepted that to extinguish a fire, water must be applied at an ample rate for the gallons per minute (gpm) to cool the Btus being produced. If we increase the Btu production, a greater gpm is typically required. Greater gpm requires the use of larger hoselines, which are more difficult to maneuver and operate, thus increasing the firefighter workload. The greater workload coupled with the reduced staffing levels significantly increases the overall work demands of firefighters and results in increased cardiovascular strain.
 |
| (2) Rehab should be provided at emergency incidents and training events. The detrimental effects of heat stress become cumulative with repeated live fire evolutions during training and, therefore, must be aggressively addressed through rehab. |
Not only has the Btu production at fires changed, but modern building design and construction techniques also have negatively impacted fire suppression. Common construction techniques designed to allow more open and flowing floor plans use materials that have great strength but fail rapidly when subjected to high heat. This design allows rapid spread of hot fire gases that result in a weakened structure and decreased time to flashover, making conditions quickly untenable for both occupants and firefighters.17
The combination of greater Btu production, the need for higher gpm, changes in the stability of structures, and fewer responding firefighters all work to increase the physical demands on personnel and compound the risk of a cardiovascular incident in individuals with underlying disease.
No “New” Money
The fire service continues to be plagued by LODDs and injuries. Over the past 10 years, on average, 86 firefighters die annually in the line of duty, and between 65,000 and 70,000 injuries are reported.18 The total cost of firefighter injuries exceeds $8 billion annually. The average firefighter injury, including workers’ compensation and backfill, costs $74,000.19
A study conducted in the Hanover Park (IL) Fire Department (HPFD), which has 55 uniformed personnel, analyzed line-of-duty injury statistics over a five-year period between 2002 and 2007. During that time period, 50 firefighter injuries occurred, ranging from minor scrapes and cuts to two significant shoulder injuries. The majority of the injuries occurred at the scene of an emergency incident or during training. In many of the cases, the firefighters had been performing physically demanding work and were likely suffering detrimental effects of heat stress. Collectively, these injuries generated 22,649 hours of workers’ compensation sick leave. Backing out the workers’ compensation insurance payments, the direct cost of these injuries (including overtime for company staffing backfill) was $770,000.20
 |
| (3) Firefighters undergo rehab at an extra-alarm apartment fire. (Photo by Diane M. Zaccard.) |
If this number is considered normal and expected, we can easily assume that every five years the HPFD spends three-quarters of a million dollars to manage line-of-duty injuries. Now the question: If many of these injuries could be prevented, could the savings be used to pay for injury and illness prevention programs? Comprehensive medical exams, fitness programs, exercise equipment, dietary programs, and incident rehabilitation teams could all be funded fully or in part by the savings garnered through a comprehensive health/injury prevention program. Additional budget dollars are rarely available to initiate these new programs, but if no “new money” is required, the available funds can likely be redirected to pay for prevention rather than the direct and indirect cost of injury or illness.
Effective Collaborations/Identifying the Resources
Because of the overall reduced staffing levels in the fire service and the cost associated with career personnel ($80,000 to $100,000 for salary and benefits),21 few departments are in a position to regularly staff and operate a rehab unit. Yet, finance deficiencies cannot be used to justify a failure to provide incident rehab services. To forgo the process and ignore the fact that incident rehab can significantly reduce the detrimental effects of heat stress and dehydration and thereby lower the risk of a cardiovascular event or injury is negligence on our part as fire service leaders. Departments should consider collaborative resources that can assist with this function. Agencies such as The Salvation Army and the Red Cross may be able to assist, depending on their local capabilities. Some communities have volunteer organizations dedicated to assisting the fire service; their members can be trained and equipped to provide rehab.
A good example is the Fire Corps team serving the HPFD. This team consists of 15 volunteers who respond on the initial alarm to all reported structure fires. All team members have completed the basic National CERT training program and have had additional specialized training on how to provide rehab. Once on scene, this team is partnered with paramedics who conduct medical assessments while Fire Corps members provide hydration, cooling, and nourishment. The team operates similarly to how a volunteer fire department functions. Members carry a radio pager that alerts them to calls in which they are due. They then respond to the station, pick up their apparatus, and report to the scene.22
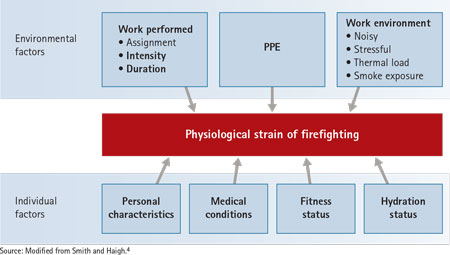 |
| Figure 1. Factors Influencing Responses to Firefighting |
The initial capital required to begin the Fire Corp program was obtained primarily through grant funding. A decommissioned ambulance was retrofitted and equipped with the supplies and equipment needed to provide on-scene rehab.23
Since the Fire Corps Rehab Response Team was first rolled out eight years ago, acceptance of field rehab has been embraced more and more. The team was originally created to serve Hanover Park and then was expanded to cover the Village of Streamwood and the Bartlett Fire Protection District.24 The team, in recent years, has started providing rehab services to all of MABAS (mutual aid) Division 12 (which covers a large portion of the western suburbs of the Chicago metro area).25 Recently, the Division has moved to a joint funding program to offset the cost of the team’s operation.
In addition, MABAS coordinated multiple trainings to provide education to firefighters on the detrimental impact of heat stress and the role of rehab. These trainings were based on scientific research and proved instrumental in getting firefighters to embrace the need for on-scene rehab. Rehab education was also added to the standing curriculum of the basic paramedic education program within the Greater Elgin Mobile Intensive Care System.
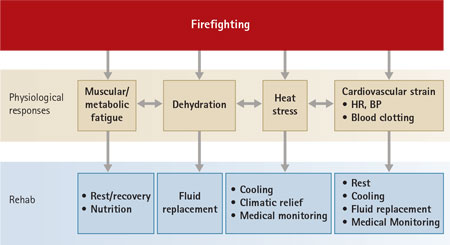 |
| Figure 2. Mechanisms by Which Rehabilitation Mitigates the Physiological Strain of Firefighting |
Firefighting involves strenuous physical work; it almost always leads to fatigue, dehydration, and significant thermal and cardiovascular strain. In severe cases, it may serve as the trigger for a sudden cardiac event in individuals with underlying cardiovascular disease. Incident rehabilitation is designed to mitigate the physiological strain of firefighting by providing rest/recovery, cooling, rehydration, and nourishment, thereby lessening cardiovascular and thermal strain and decreasing the risk of injury on the fireground. Given all the important benefits of rehab, we must think more broadly and remember that who provides the rehab is not nearly as important as the fact that rehab is being provided to those in need.
It is imperative that fire service leaders begin developing systems in which on-scene rehab is readily available and part of the initial response plan. The case study of how Hanover Park tackles this issue is only one example of many models that have proven to work well in providing this unique, but vital, need of the fire service.
Endnotes
1. Fahy, RF, PR LeBlanc, and JL Molis. (2014). Firefighter Fatalities in the United States-2013. Quincy, MA: National Fire Protection Association.
2. Kales, SN, ES Soteriades, CA Christophi, and DC Christiani. (2007). “Emergency Duties and Deaths from Heart Disease among Firefighters in the United States.” The New England Journal of Medicine 356(12), 1207-1215.
3. Smith, DL, DA Barr, and SN Kales. (2013). “Extreme Sacrifice: Sudden Cardiac Death in the U.S. Fire Service.” Extreme Physiology and Medicine 2(1), 6; doi: 1186/2046-7648-2-6.
4. Smith, DL and C. Haigh. (2006). “Implementing Effective On-Scene Rehabilitation.” Fire Engineering, 175-183.
5. Smith, DL, TS Manning, and SJ Petruzzello. (2001). “Effect of Strenuous Live-Fire Drills on Cardiovascular and Psychological Responses of Recruit Firefighters.” Ergonomics 44, 244-254.
6. Smith, DL, K Dyer, and SJ Petruzzello. (2004). “Blood Chemistry and Immune Cell Changes During 1 Week of Intensive Firefighting Training.” Journal of Thermal Biology 29, 725-729.
7. Smith, DL, Petruzzello, SJ, Chludzinski, MA, Reed, JJ, & Woods, JA. (2005). “Selected Hormonal and Immunological Responses to Strenuous Live-Fire Firefighting Drills.” Ergonomics 48, 55-65.
8. Smith, DL, GP Horn, SJ Petruzzello ,G Fahey, J Woods, and B Fernhall, B. (2014). “Clotting and Fibrinolytic Changes after Firefighting Activity.” Medicine and Science in Sport and Exercise 46(3), 448-454.
9. Brown, JB, A Bennett, PA Derchak, M DeMarzo, and S Edwards. (2006). Health and Safety Guidelines for Firefighter Training: Center for Firefighter Safety Research and Development. College Park, MD: Maryland Fire and Rescue Institute, University of Maryland.
10. Espinoza, N and M Contreras. (2007). Safety and Performance Implications of Hydration, Core Body Temperature, and Post-Incident Rehabilitation. Irvine, CA: Orange County Fire Authority, Wellness, and Fitness Program.
11. Horn, GP, J DeBlois, I Shalmyeva, and DL Smith. (2012). “Quantifying Dehydration in the Fire Service Using Field Measures and Novel Devices.” Prehospital Emergency Care 16(3), 347-355.
12. Fernhall, B, CA Fahs, G Horn, T Rowland, and D Smith. (2012). “Acute Effects of Firefighting on Cardiac Performance.” European Journal of Applied Physiology 112(2), 735-741.
13. Soteriades, ES, DL Smith, AJ Tsismenakis, DM Baur, and SN Kales. (2011). “Cardiovascular Disease in U.S. Firefighters: A Systematic Review.” Cardiology in Review 19(4), 202-215.
14. Horn, GP, S Gutzmer, CA Fahs, CA, SJ Petruzzello, E Goldstein, GC Fahey, B Fernhall, and DL Smith. (2011). “Physiological Recovery from Firefighting Activities in Rehabilitation and Beyond.” Prehospital Emergency Care 15(2), 214-225.
15. National Fire Protection Association. (2014). Fire Department Calls [Annual Report]. Quincy, MA: National Fire Protection Association.
16. Kennedy, PM and KC Kennedy. (2003). Flashover and Fire Analysis – a Discussion of the Practical Use of Flashover Analysis in Fire Investigations. Proceedings from the 10th International Fire Science and Engineering (Interflam) Conference, Interscience Communications, Ltd., London, July 5-7, 2004, 1101.
17. Jaehne, R, D Clark, J McCastland, J Norman, and D Smits. (2007). Street Smart Modern Construction Considerations for Firefighters. Retrieved from www.fsi.illinois.edu: http://www.fsi.illinois.edu/content/virtual%20campus/VC_pfd/ff%20tactics%20decision%20mkg%20ltwgt%20const%202007final_1.pdf.
18. Karter Jr., MJ and JL Molis. (2014). Firefighter Injuries in the United States-2013. Quincy, MA: National Fire Protection Association.
19. TriData Corporation. (2005). The Economic Consequences of Firefighter Injuries and Their Prevention. Final Report (NIST GCR 05-874). Retrieved from National Institute of Standards and Technology:
20. Haigh, CA. (2006). Reducing Fire Ground Injuries Due to Heat Stress at Hanover Park Fire Department (Accession No. 124023/OCLC Record No. 47589881/Call No. 39977). Emmitsburg, MD: National Fire Academy – Learning Resource Center.
21. W. C. Bednarek, Hanover Park human resource director, personal communication, May 22, 2015)
22. Citizen Corps – CERT. (2009). http://www.citizencorps.gov/cert/about.shtm.
23. NVFC: Fire Corps. (2009). http://www.firecorps.org.
24. Hanover Park Fire Department. (2007, November 11). Fire Corps (Departmental Policy Ch. 100, Section 048). Village of Hanover Park, Illinois: Hanover Park Fire Department.
25. MABAS Division 12. (n.d.). http://mabasdiv12.com/.
CRAIG A. HAIGH, a 32-year veteran of the fire service, is chief of the Hanover Park (IL) Fire Department and a field staff instructor with the University of Illinois Fire Service Institute. He has managed volunteer, combination, and career departments; implemented intermediate and paramedic services; and developed a variety of courses for the fire service. He is an FDIC International H.O.T. instructor. He has a BS degree in fire and safety engineering and an MS degree in executive fire service leadership. He is a nationally certified paramedic and a graduate of the Executive Fire Officer Program.
DENISE L. SMITH, Ph.D., is professor of health and exercise sciences at Skidmore College in Saratoga Springs, New York, and a research scientist at the University of Illinois Fire Service Institute. She is co-author of the textbook Exercise Physiology: For Health Fitness and Performance, currently in its 4th edition, and Advanced Cardiovascular Exercise Physiology. Her research is focused on the physiological effects of firefighting, particularly the cardiovascular strain associated with the combination of heavy physical work and heat stress that firefighters routinely encounter. Her research has been funded by several national agencies, including the Federal Emergency Management Agency’s Assistance to Firefighter Grants, the National Institute for Occupational Safety and Health (NIOSH), and the Department of Defense. She has published more than 50 peer-reviewed scientific articles, and she often shares the findings of her research in the fire service. She conducts fatality investigations related to cardiac events for the NIOSH Firefighters Fatality Investigation Program and is a member of the National Fire Protection Association technical committee on Fire Service Occupational Health and Safety.
FIREFIGHTER HYDRATION DURING REHAB
CAN ADEQUATE REHAB PREVENT FIREFIGHTER DEATHS?
REHAB UNITS AT WORK
Fire Engineering Archives

