By Jeff Belczak
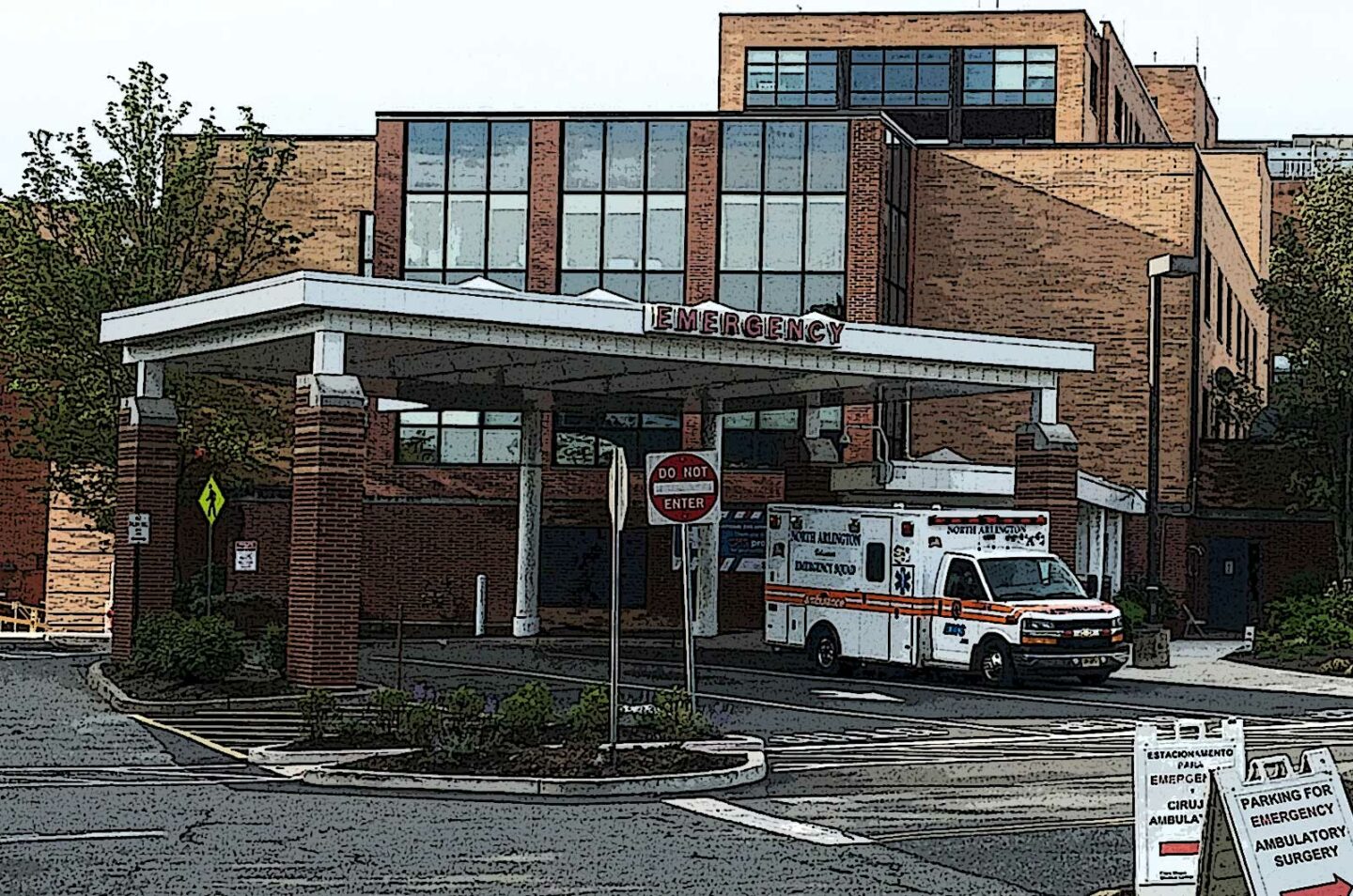
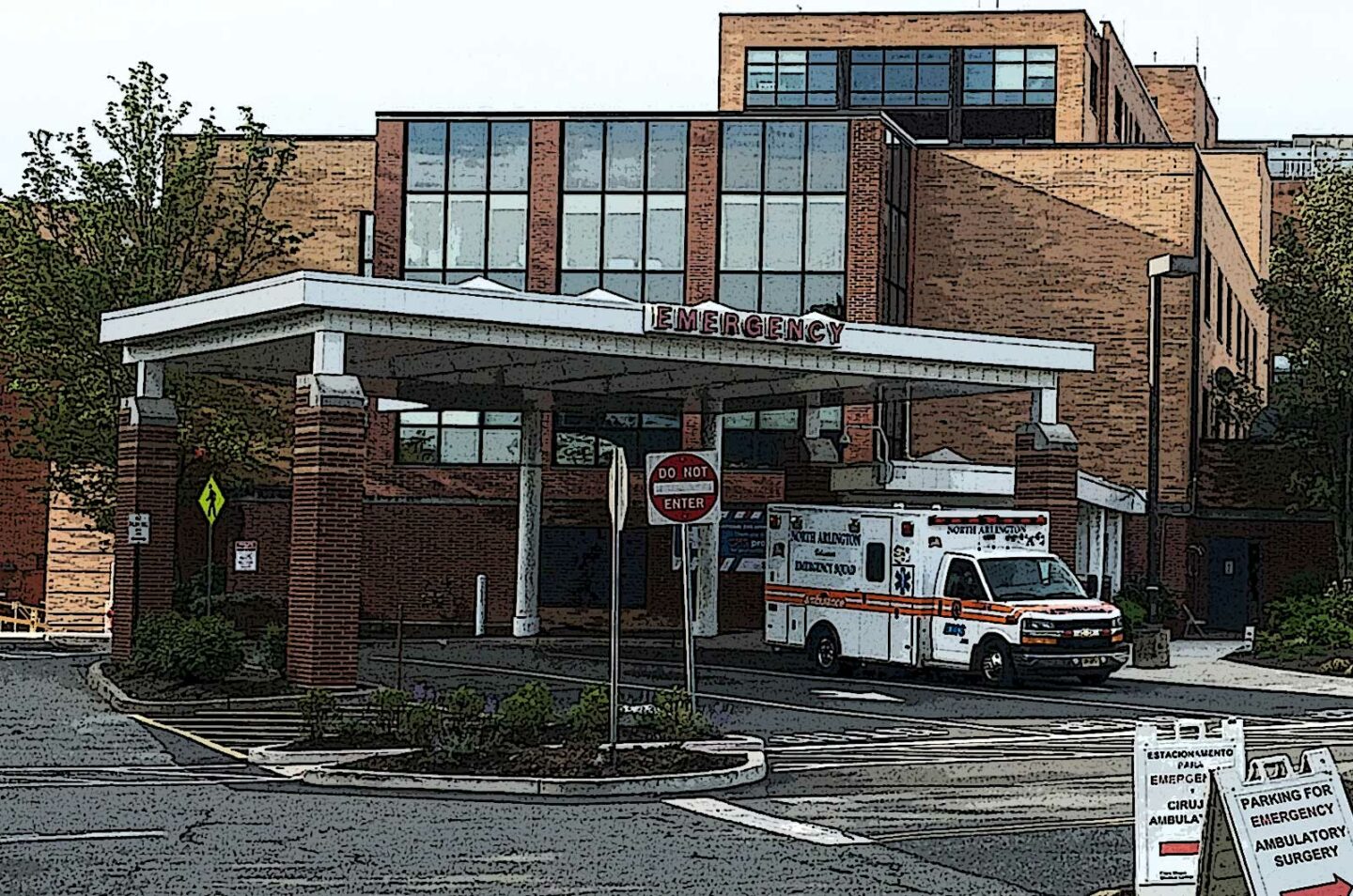
Firefighters are trained and equipped to handle anything thrown at us, but COVID-19 has presented many new challenges to our emergency responders in the field. These include a wide array of new and challenging medical cases, complex decontamination practices, and expanding challenges with target hazards in first-due response areas. Responding to healthcare occupancies of all varieties and sizes for fire alarms, odor investigations, and the occasional fire is not a new task for many fire departments, but the unique and ever-changing landscape of those occupancies present new realities and challenges for us to effectively do our job. In this discussion, healthcare occupancies are those facilities where staff are assigned the duty of responding to fire emergencies to protect those that are not capable of self-preservation (taking care of themselves). This may include hospitals, nursing homes, behavioral health inpatient treatment centers, or surgery centers.
RELATED
Hospital Fire Safety: RACE for the Extinguisher and PASS on It!
Fires in Hospitals and Nursing Homes: Be Prepared for the Unexpected
On a normal day, healthcare facilities are filled with sick folks of varying health conditions. We must understand that our response alone to these occupancies for even minor incidents can create additional complications for those that seek medical care and preservation. Firefighter personal protective equipment (PPE) may be stained, dirty, or contaminated from previous runs or even from sitting in unsterile locations. When we enter these facilities, we must both protect ourselves from individuals with a wide array of medical issues and protect those in fragile medical states from us. Healthcare facilities in general are far more sterile than our apparatus, apparatus bay, and even our refrigerators.
Healthcare facilities alone can be a challenge in terms of size, complexity, and mere scope of services. We perhaps don’t routinely deal with these elements, but because of the COVID-19 pandemic, each facility is changing the layouts and landscapes of the property along with procedures for fire response. In some cases, and as local statistics change (for better or worse) involving COVID-19, sweeping changes may occur overnight. Fire departments must be responsive to them and understand how those changes affect our response capability and plans. These changes may include the facilities’ internal response to fires, the available access for apparatus and firefighters, changed floor plans, evacuation changes, and change in services for each location in the facility, to name just a few.
Healthcare Staff Response During a Pandemic
The premise behind fire emergency response in healthcare is that the healthcare staff perform many crucial life safety functions, many times before fire department arrival. These plans are site specific and may include patient evacuation, control of medical gases (oxygen, nitrogen, medical air, vacuum, nitrous oxide, and anesthetic gases), and even control of small fires, among others. With staff dealing with COVID-specific patients in special protective wards, PPE shortages, and large numbers of personnel working from home, the facility may have less staff than normal to respond and handle those crucial functions. Facilities are also taking drastic measures to limit cross contamination of staff (to protect patients and staff) from floor to floor by reducing potential staff response. As a result, the facility fire plans may have been altered or drastically changed, and that can have an immediate impact on life safety. You’ll need to determine if their facility plans have been altered and which responsibilities you may need to plan for or even handle, some of which you may not be currently familiar with. Start by determining the number of inpatients who are not capable of self-preservation. This number will change daily but the facility should be able to give you a count for planning purposes. Not every floor or wing of a facility will have patients that can’t assist or help with their own evacuation, either by walking or in wheelchairs.
When assisting with evacuation, there are four traditional stages that healthcare facilities use. They include shelter-in-place, horizontal evacuation, vertical evacuation, and building evacuation. For a vast majority of fire emergencies, you can expect patients to be sheltered-in-place, meaning the patients are kept in their room (behind a closed door) or evacuated horizontally past the nearest smoke barrier wall. Smoke barriers are physical barriers constructed of sealed walls and doors that are designed to isolate portions of the facility and stop the transmission of smoke in case of fire. Smoke barriers are generally delineated by a set of cross-corridor doors that automatically close upon activation of the fire alarm system. With the increase of ventilator patients and the need for additional patient care capacity, corridors are being used to accommodate that surge. During a fire emergency, these patients cannot be sheltered-in-place as they are not located in a room so these patients would automatically be evacuated horizontally into an adjoining smoke compartment.
When your crew arrives on the fire floor, expect corridors to have greater congestion, making it difficult to stretch a line or investigate. Additionally, all the while you will be moving past patients receiving advanced medical care. As you can imagine, the more critical the patient, the more hands needed to help with that overall evacuation. With an influx of ventilator-dependent patients, the number of patients requiring direct specialized assistance can be significantly greater than usual, thus requiring more help with evacuation. In general, a single staff member may be able to assist with evacuating several patients simultaneously, whereas ventilator and ICU patients may need upwards of six or more people to successfully move each patient. Fire department personnel may be the extra hands needed to assist with evacuating those patients and, as you can imagine, time is of the essence. This may cause you to increase the initial response, upgrade to additional alarms (with a confirmed fire or odor of smoke), or reallocate resources traditionally assigned to handle other tasks (ventilation, elevator control, and so forth).
Fire Apparatus Access: Temporary Exterior Facilities
One of our first priorities as the responding fire department is getting our apparatus in and entering the building. Your department may have standing orders for where apparatus is to park, what assignments to handle, and specific locations that firefighters ought to enter the building during alarms. This can include apparatus positioning on different sides of the building to best use the aerial to access upper floors or to hook up to fire department connections. As facilities struggle with the growing realities of the pandemic, additional resources are being called in to assist. This can include trailers for temporary morgues, bulk supplies, decontamination services, temporary triage and care tents, and bulk oxygen and emergency power trailers. All of these may be occupying the valuable space we normally use for our fire apparatus. Getting apparatus to the site may not be ideal, but with the proper planning, it may still be effective. If procedures call for quarterly preplanning of target hazards, you may need to increase the frequency of those visits to weekly, daily, or even per shift to make sure you’re effectively able to respond.
Firefighter Entry
Our apparatus positioning and size of the facility will affect our ability to quickly enter the building. A large portion of facilities on some level are dedicated to medically screening all individuals that enter their buildings, whether it be outpatients, visitors, and even staff. To do this, they have locked all doors on the campus from anyone trying to enter except for one main entrance (egress shouldn’t be affected but plan accordingly). Consider that if a facility has 100 exterior doors for access spread out over five acres, only one main entrance may now be accessible. At that location, facility staff have added triaging stations which are designed to question every individual that enters the building to determine their current health status and even to take their temperature. The results of that screening may or may not allow an individual to enter, and that could include firefighters. You’ll want to understand the expectations that the facility has for your personnel when entering during a fire call. Of course, this will be dictated by the type and location of the emergency, and both groups need to understand each other’s concerns, access needs, and timing. Work with them so they are prepared to question and scan 12 or more personnel right away. Will they give you alternate access to other parts of the building? Who can get you that access? What are the potential complications of entering for each (floor plan changes, etc.)? Now is the time to figure out these potential factors.
As we continue moving forward with this pandemic, the need and type of PPE may vary when entering healthcare facilities. This can range from a simple face covering to full self-contained breathing apparatus (SCBA) use, gowns, booties, or eye protection. At the time of dispatch, you may not know where in the building you will be heading. Consider the need to adjust standing orders for use and type of PPE prior to dispatch specifically for healthcare facilities. A simple odor investigation may take you to multiple floors and covering spaces with COVID-positive patients. As the odor goes, so do we, and we can’t be heading back to the rig to get a different type of PPE. Depending on the type of emergency and needs of the facilities fire plan, consider limiting the amount of personnel in the building or on a particular floor. Stage crews in low-risk areas to allow for rapid deployment if needed. Limiting high-risk exposure to our personnel can serve many potential functions, including reducing the need for PPE (some departments may face shortages) and ensuring our staffing levels are met (in the future). Working and gaining a relationship with facility personnel is invaluable. Together, you may determine that the risk of sending fire department personnel to investigate a smoke detector activation with no signs of smoke or fire may be greater than allowing the facility staff to investigate on their own (for certain areas). Having fire department staff enter COVID-19 units with full PPE and SCBA to simply investigate will require the need for decontamination prior to leaving the unit as facility staff would do the same with their PPE. You will not be able to leave a COVID unit without taking all your gear off to limit the potential spread throughout the facility. This can either involve on-site decon or packaging and transport of potentially infected fire gear and SCBA via fire apparatus back to the station. All this needs to be by department policy and discussed with healthcare staff in advance. If you do plan on entering, work with facility personnel to determine if you’ll be using their PPE or yours. Will they allow gowns to be used over turnout gear, or respirators that you haven’t been fit tested to? Again, now’s the time to make these determinations.
Changing Floor Plans for Temporary In-Patient Care Overflow Areas
If you haven’t already performed an in-depth preplan of your area healthcare facility, it may be too late for the unplanned visit, but know the interior layout of the building may have changed in some fashion. In some instances, floor plans are changing almost daily to meet or prepare for the surge and varying challenges presented by the COVID patients or to move services to accommodate that surge. Last week, you may have responded to the auditorium on the fourth floor for an electrical burning odor but overnight that auditorium was converted to handle 15 acute care patients, a makeshift morgue, or even a room under negative pressure for COVID-only ventilator patients. You may arrive to stretch on a reported fire on that same fourth floor only to find out a temporary wall has been constructed for an anteroom used for PPE gowning. That temporary wall then separates an entire wing, a block of rooms, or even a single room from the rest of the floor. Instead of a physical hard surface wall with a side-hinged door, you may find a plastic partition with magnets, zippers, or even velcro, all of which may make things difficult to evacuate patient and get access. These changes may even present orientation issues.
Depending upon the patient care or service being provided, different ventilation techniques (positive or negative) may be used for certain areas to limit cross contamination for patients, visitors, staff, and sterile equipment. With the increase need to surge hospital capacity, temporary compartments are being built to enable a wing or part thereof to be under negative or positive pressure. If power is going to be secured or ventilation affected, firefighters need to understand the affects that it may provide on the safety of everyone. Prior to securing power or changing air flows (via ventilation), consult facility maintenance, safety, or clinical staff. This can make all the difference between spreading harmful contaminants normally contained to other parts of the building.
It may be too late to make that unplanned visit to your local facility but there are several ways you can stay involved. Stay in daily communication with the local safety, emergency preparedness, or engineering departments. They can provide you with a list of all locations housing COVID patients, a drawing of each floor with a quick overview of floor plan changes, services being moved, changes in utilities, or temporary medical equipment put into operation. This also serves as the starting point for the sharing of information so they can adapt to your needs even as you adapt to their ever-changing landscape.
You may be prepared to stretch a hoseline in a large, multi-story building, but the mental aspect and timing of that stretch or search may be more difficult as things may change daily. As the battle of COVID-19 is waged in the streets by emergency responders, the ever-changing landscape of our healthcare facilities can present many new and unique challenges for the very same individuals. The mental preparedness for these new challenges may be more difficult than ever before, so stay active in your first due, stay vigilant to daily changes, and communicate with hospital representatives.
Jeff Belczak is a 24-years veteran of the fire service and is a captain with the Baldwinsville (NY) Fire Company. He is a graduate of the Fire Protection and Safety Engineering program at Oklahoma State University and a regional fire protection Engineer with the Department of Veterans Affairs for the New York/New Jersey region.

