
“There comes a point where we need to stop just pulling people out of the river. We need to go upstream and find out why they’re falling in.” ― Desmond Tutu
It’s common knowledge that first responders are exposed to trauma at higher rates than the general population, and it is no surprise that exposure to trauma increases one’s risk of developing behavioral health disorders, including depression, anxiety, and post traumatic stress disorder (PTSD). According to a 2018 Substance Abuse and Mental Health Services Administration (SAMHSA) report, first responders were estimated to have a 30% chance of developing a behavioral health condition, compared to the general population, who are only 20% likely to develop such conditions (Substance Abuse and Mental Health Services Administration, 2018). For this reason, first responder organizations have adopted models to support members of their organizations, such as critical incident stress management (CISM) teams, chaplaincy, peer support, and employee assistance programs. However, in their efforts to react to trauma and poor health outcomes, many organizations have failed to prepare and support their members long before they find themselves in need of these reactionary resources. This article will explain why we must move upstream and focus our resources and energies on helping to develop more prepared responders.
RELATED
- Sleep: A Missing Link to Cancer Prevention
- Addressing Internal Conflict to Understand Suicide
- Dispelling Some Common Myths About Suicide
- Can Peer Support Prevent Firefighter Suicide?
Critical incident stress debriefing (CISD), which is considered a best practice, has been used since 1983 and is a component of CISM (Mitchell, Sakraida, & Kameg, 2003). Despite its popularity and continued use, the efficacy of CISD has had mixed results. In his book, Surviving Survival, Author Laurance Gonzalez (2012) shared:
This technique of forcing people to talk after they experience trauma is known as CISD and it’s been shown to be ineffective and even harmful. In fact, a lot of the patients committed suicide. This does not mean that keeping trauma secret is the best approach. It means that writing about your experience or talking with friends and family only when you’re ready are often better than being forced to unburden yourself in a formal, professional setting (pg. 31)
Moreover, while many of the commonly used resources serve to assist first responders who have been impacted by trauma, few help the responder better prepare to handle the stress inherent in life and in their careers through the development of resilience. In her course Stress Injury Awareness, Laura McGladery discussed the responder continuum (see appendix B), and explained that while there are numerous treatments available for a responder who becomes severely impacted by trauma, it is far better to teach them ways to manage stress before they reach that point. The continuum is a detection tool first created by the U.S. Marine Corps to be used as a self-assessment of how an individual soldier is managing stress. In explaining its usefulness, McGladery used the analogy of a diabetic who ends up in ICU due to lack of self-care: while the doctors can treat the diabetic and eventually help that individual heal, if the patient would have practiced self-care and connected with resources long before ending up in crisis, the paitent would not have become disabled and in ICU in need of such complex resources.
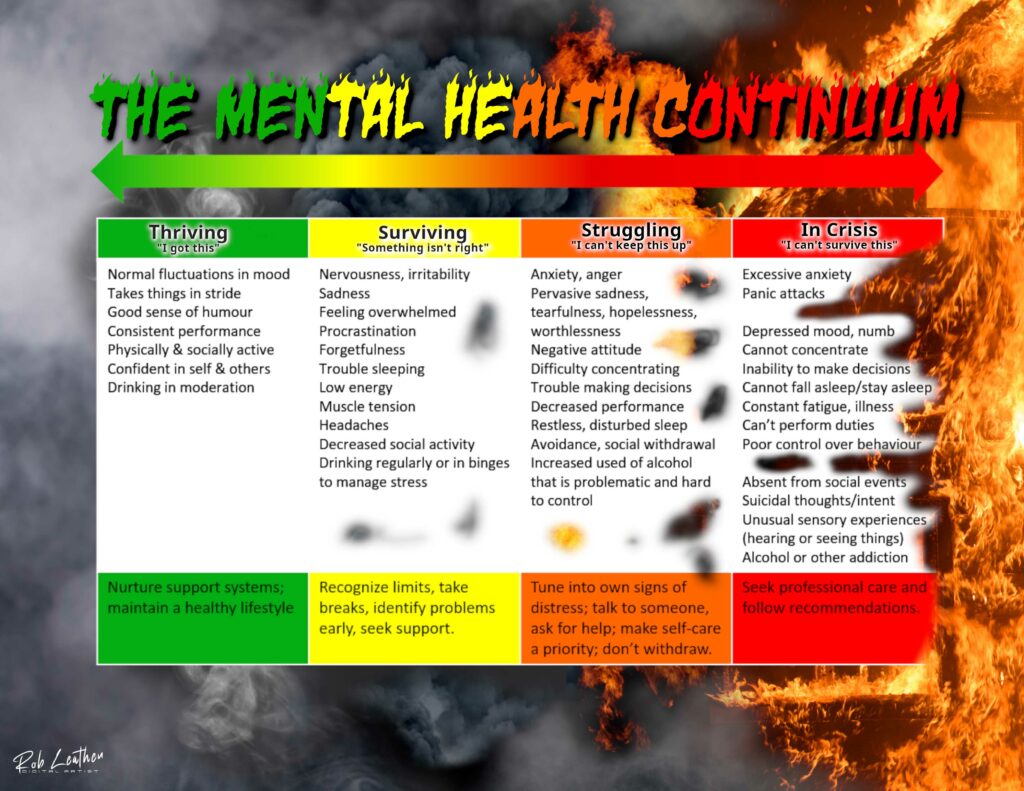
A self-assessment tool such as the stress continuum better helps the responder recognize when they are reacting to stress, and when self-care may be useful. This works in a manner similar to a diabetic who recognizes symptoms of low or high blood sugar and implements self-care to stay healthy. Additionally, that diabetic knows to reach out to professional care when their self-care tools are no longer working. Just like the key to improving physical health lies in prevention, the key to improving first responder mental health also lies in prevention, which should occur long before exposure to trauma, stress, or a critical incident. Unfortunately, this is an area where many fire departments are lacking in education and resources for their members.
First responder organizations must focus on ensuring their members are safe, healthy, prepared, and resilient. A simple definition of safe is protected from harm. To ensure the safety of our members, leaders must take a systems approach to protecting their members from developing behavioral health disorders. This means, we must step onto the proverbial balcony and recognize factors outside of call responses that may contribute to poor outcomes.
Dr. Janet Savia was able to do this while completing her dissertation on first responder suicide in 2007. What she found was that our call responses are just one variable that impact our mental health. Interestingly, she found that we often believe the true sources of our pain are insignificant compared to the real problems facing others, and because of this, we are ashamed of sharing our struggles (Savia, 2008). However, she discovered that it is often these things that we believe are insignificant that build into a true crisis and can lead to suicide. A common example she found was bullying and disconnection. Writing in his book The Beauty of a Darker Soul, Joshua Mantz (2018) notes that trauma is complex and cumulative, and our responses are a result of everything that has come before –our early life experiences, how we were raised, and our relationships. They are all interrelated; unresolved traumatic experiences create cracks in our foundation, and if we move forward without addressing the cracks, we build on a shaky foundation (Mantz, 2018). Therefore, sometimes insignificant events can cause severe reactions. To understand the sources of our trauma, we must allow ourselves permission to explore, recognize, and validate our experiences. This is most effectively and safely accomplished in the presence of a trained trauma therapist (Mantz, 2018).
Interestingly, the research has demonstrated that support from supervisors is the strongest predictor of decreased PTSD severity for first responders (Stanley, et al., 2019). In looking to improve the safety of first responders, we must ensure our supervisors are prepared to support their members and are aware of the impact of their support. For example, trusted leaders who encourage the use of mental health resources predict a greater usage of these resources (Stanley, et al., 2019). Imagine the impact of a respected leader who models utilization of therapy and counseling?
Additionally, it is not enough that the supervisors are prepared to support their subordinates. We must ensure our first responders are prepared to handle the stress inherent in our occupations. Preparation requires that our responders understand the variables that predict their ability to withstand exposure to trauma so that they can experience post traumatic growth (PTG) as opposed to PTSD. These variables all support the resilience of our first responders. One way to bolster our resilience is by increasing our bandwidth through activities that train the prefrontal cortex and limbic system of the brain (Munsey, 2018). Because we have a limited capacity for the “stuff” we can deal with before reaching our breaking point, we must recognize how to increase our threshold (Munsey, 2018). Any activity that shuts down the sympathetic nervous system increases our bandwidth, which is measured by heart rate variability (HRV) (Munsey, 2018). These activities include sleep, yoga, breath work, mindfulness, rest, play, gratitude, laughter, journaling, and time with loved ones (Munsey, 2018).
Rapid Intervention Team: Is Your Commitment Sufficient?
Building more prepared, healthy, and resilient first responders requires educating them on the importance of increasing their bandwidth and ensuring they have the tools necessary to be successful at these activities. After experiencing a line-of-duty death in 2011, the Asheville (NC) Fire Department recognized the need to improve the resilience of their members and incorporated an eight-week mindfulness-based stress reduction course for their recruits (Bettencourt, 2022). This is just one example of increasing the safety of first responders through bolstering their resilience so that they can be better prepared to handle stressful situations. All of the actives designed to increase HRV also help the responder move back to a healthy position on the responder stress continuum. By educating responders on how to recognize when they are reacting to stress and then providing them with tools to improve their HRV, we become successful at helping them remain healthy and able to continue functioning without the need for complex resources.
Firefighters and other first responders undergo evaluation to ensure they are healthy before hire. These evaluations often ensure the members are illness and disease free so that they can benefit the organization. If it is so important that we hire healthy first responders, shouldn’t it be equally important to ensure our first responders remain healthy throughout their career? There are several biomarkers for evaluating health. These include white blood cell activity, HRV, testosterone, cortisol, and quality of sleep. Sleep is a critical component of health because inadequate sleep has been found to lead to cancer, heart disease, early mortality, PTSD, diabetes, obesity, depression, risk taking, cognitive impairment, and reduced learning capacity (Marks, Callahan, & Grill, 2019). Moreover, research consistently returns findings indicating that improved sleep is the most robust variable that improves HRV (Walker, 2017) If there was just one variable that could improve the preparedness, safety, resilience, and health of first responders, it would be quality sleep.
However, many organizations fail to address resilience through preparation, and rather focus efforts solely on postincident debriefings, chaplaincy, and psychological intervention. Yet, if we continue to fail at ensuring our members are prepared to respond to traumatic events, we will continue to fail at developing resilient members. By failing to develop resilient members, we will continue to be forced to rely on postvention. This the equivalent of relying on ICU to ensure members are healed after medical crisis as opposed to preventing them from ever ending up in the ICU.
Where do we start?
- Leadership that models resource utilization (therapy)
- Leadership that models the importance of self-care
- Encouraging members to have strong support networks and relationships
- Encouraging rest and play
- Having an enjoyable hobby outside of work
- Implementing an eight-week mindfulness-based stress reduction program
- Learning everyday mindfulness practices to include gratitude and journaling
- Education on sleep hygiene and encouraging good sleep practices
- Station design that incorporates sleep optimization
- Education on tactical napping
References
Bettencourt, J. (2022, August 9). (D. Ali, Interviewer)
Gonzales, L. (2012). Survivng Survival: The art and science of resilience. New York: W.W. Norton & Company.
Heifetz, R., & Linsky, M. (2017). Leadership on the Line. Boston : Harvard Business Review Press .
Mantz, J. (2018). The Beauty of a Darker Soul: Overcoming Trauma through the Power of Human Connection. Austin: Lioncrest.
Marks, M., Callahan, P., & Grill, M. (2019). A Community of One: Building Social Resilience. Pennwell: Tulsa .
McGladery, L. (2020, August ). Responder Stress Injury Awareness. Boulder , CO.
Mitchell, A., Sakraida, T., & Kameg, K. (2003). Critical incident stress debriefing: implications for best practice. Disaster Management & Response, 46-51.
Munsey, R. (2018). Master your mind: Accomplish anything and become a more significant human. Boyce: Strong House Press .
Savia, J. (2008). Suicide among North Carolina professional firefighters. Disseration Abstratcts International.
Stanley, I., Hom, M., Chu, C., Dougherty, S., Gallyer, A., Spencer-Thomas, S., . . . Joiner, T. (2019). Perceptions of belongingness and social support attenuate PTSD symptom severity among firefighters: A multistudy investigation. Psychol Serv, 543-555.
Substance Abuse and Mental Health Services Administration. (2018). First Responders: Behavioral Health Concerns, Emergency Response, and Trauma. District of Columbia: Supplemental Research Bulletin.
Walker, M. (2017). Why We Sleep . New York: Scribner.
Dena Ali is a battalion chief in the Raleigh (NC) Fire Department with 15 years of service. She has a master’s in public administration from the University of North Carolina at Pembroke

