
A Responsibility for EMS Agencies
By Tanner Smida
A man is outside washing his car on a warm spring day. Suddenly, he collapses next to the vehicle and lies motionless in a puddle of sudsy water. A neighbor who happened to witness the fall calls 911 and reports an unresponsive 60-year-old male who is not breathing. She does not know CPR, and despite the dispatchers attempt to talk her through this procedure, she does not provide chest compressions. Within two minutes of the arrest, a volunteer firefighter screeches to a halt at the curb in his personal vehicle, rushes to the victim’s side, and begins to perform CPR. Another minute passes before the local fire department’s emergency response vehicle arrives with an AED. Six shocks are delivered before EMS arrives on scene without sustained restoration of a perfusing rhythm. The patient is in asystole by the time intravenous access is established, and the decision to terminate efforts is made 40 minutes following the initial arrest.
In theory, the chances of a successful outcome for this resuscitation were high. Emergency services were contacted immediately, and BLS resuscitation was initiated while the patient was still in the electrical phase of the arrest and presenting with a shockable rhythm. In this case, things ended poorly, but steps can be taken to ensure better future outcomes in similar scenarios.
RELATED
Rialto Fire Department Changes the Paradigm of Cardiac Arrest
Seven Tools Result in Dramatic Improvements in Cardiac Arrest Outcomes in Rialto, Calif.
We operate in the rust belt of Pennsylvania, an impoverished area with little municipal funding for emergency services and understaffed EMS agencies that cover post-industrial towns with a declining population density. In terms of demographics, the population of our service area has a high proportion of elderly citizens, suffers from a heavy burden of chronic respiratory disease, and is socioeconomically deprived. Bystander CPR rates are low, and publicly accessible defibrillators are largely unavailable. In essence, we find ourselves in the midst of a perfect storm for poor cardiac arrest outcomes. Time is working against us as well. Because of the aforementioned geographic and economic restrictions, response times for EMS are typically greater than the four-minute target set by National Fire Protection Association 1710, Standard for the Organization and Deployment of Fire Suppression Operations, Emergency Medical Operations, and Special Operations to the Public by Career Fire Departments (7.3-minute median response time for cardiac arrest).
However, volunteer fire departments within the jurisdictions we serve arrive on scene under this critical threshold for the majority of “priority dispatches” (i.e. unresponsive patients, motor vehicle accidents, major trauma, etc.) While the six shocks delivered in the scenario above constitute a clear outlier, it is not uncommon for an ambulance staffed with an ALS provider to arrive on scene of a cardiac arrest after two defibrillation attempts have already occurred. This is due to several factors, including the reduced service area that volunteer departments cover compared to EMS (roughly one-third), and the distribution of members within their community, which gives these departments a high probability of having a member in closer proximity to the victim of a medical emergency when it occurs than the nearest EMS crew. In addition, given that the number of EMS agencies is declining nationwide, the time it takes for a sick patient to receive definitive care by a specially trained prehospital provider is at risk of increasing. Due to the rapid response time of volunteer fire-based first responders, it is my contention that these individuals are an underutilized resource that have the potential to provide incredible benefit to the practice of prehospital resuscitation in some communities. Rapid intervention by these volunteers is of additional importance when it is considered that rural or semi-rural areas may be a great distance from high level post-resuscitation care (i.e. PCI, therapeutic hypothermia, etc.).
In the case of cardiac arrest victims, every second is critical. This group of patients in particular cannot afford to wait seven minutes for interventions to be performed by paramedics and EMTs. One often cited estimate suggests that a patient’s chances of survival decrease by approximately 10 percent for every minute that BLS interventions are delayed, which emphasizes the critical need for rapid intervention [1]. It has been well established in the literature that early BLS resuscitation and defibrillation are correlated with neurologically intact survival [1-5]. Given that about 40 percent of these fortunate survivors achieve a return to a perfusing rhythm after the first or second shock delivered by prehospital providers, it is incredibly important to ensure the maximal effect of the first shocks that are delivered before the arrival of EMS. Evidence-based “cardiocerebral” resuscitation (CCR) protocol implementation hold the promise of furthering this goal and improving early resuscitation success rates [6, 7].
CCR emphasizes 1) pre-shock compressions augmented by 2) passive oxygenation and BLS airway management in addition to 3) immediate post-shock compressions for each defibrillation attempt. Developed by Bobrow, Ewy, and others based on research conducted by the resuscitation group located at the Sarver Heart Center in Arizona, this mode of resuscitation has been conclusively shown to improve outcomes from sudden cardiac arrest in clinical studies [6, 8-11]. Despite the proven success of this protocol and adoption of portions of these practices into ACLS guidelines, I have personally observed a lack of knowledge regarding the effectiveness of these methods, specifically among BLS providers such as volunteer firefighters.
Interviews conducted with 12 firefighters from four different volunteer-based departments yielded a common theme in their descriptions of the early phase of cardiac arrest resuscitation. Upon arriving on scene, the firefighters invariably reported initiating defibrillation as soon as the AED pads were able to be attached, and beginning bag-valve mask (BVM) ventilation utilizing a 30:2 compression to ventilation ratio as soon as a pair of hands were available. All of the providers I interviewed also described the performance of a pulse check immediately following the first defibrillation attempt. The following modifications of these early steps in cardiac arrest resuscitation using tools that are readily available to volunteer firefighters can improve first shock success rates and increase neurologically intact survival.
1. First, it is important to emphasize the performance of a full cycle of pre-shock compressions prior to the first defibrillation. In the first minutes following an arrest, blood shifts from the high pressure, arterial portion of the vasculature to the venous side, causing the right side of the heart to increase dramatically in size [12, 13]. The volume increase on the right side of the heart contributes to pericardial restraint and tamponade, and if this accumulation of blood is not redistributed by the performance of 200 high quality compressions, even successful defibrillation will be unable to restore the ability of the heart to pump enough blood to be self-sustaining and prevent recurrence of arrest. One study conducted in Arizona revealed a 0/21 first shock success rate with a median response time of six minutes, 27 seconds and no CPR before defibrillation [14]. This provides validation for the benefit of pre-shock compressions that has been reported in the medical literature using both animal models of sudden cardiac arrest [13, 15, 16] and clinical studies of arrest victims [17, 18]. During this approximately two-minute period, AED pads should be placed and passive oxygenation should be initiated.
2. Passive oxygenation entails the placement of a non-rebreather mask over the arrest victim’s mouth and nose at a flow rate of 15 L/min while compressions are performed. The changes in pressure inside the patient’s chest that occur with each compression (an increase with every downstroke and a decrease with chest wall recoil) cause air to be cyclically forced out of and pulled into the patient’s airway, which provides adequate oxygenation for up to 16 minutes following the initial arrest. Using this method of oxygenation also eliminates the need for BVM ventilation, which has been shown to increase intrathoracic pressure. Increased pressure inside the chest decreases preload by slowing return of blood to the heart, which reduces the efficiency of compressions. Use of BVM ventilation early in the resuscitation at a 30:2 ratio is also incorrect, as it has been conclusively shown in the literature that any pauses, even as brief as those for ventilation, have a significantly negative impact on intra-arrest hemodynamics [19]. Studies have also shown that prehospital healthcare providers, when confronted with a stressful situation such as a cardiac arrest, ventilate at three times the guideline recommended rate [20]. In addition to impacts on intrathoracic pressure, this hyperventilation can cause gastric inflation, which frequently leads to vomiting. If vomit contaminates the airway, this both impedes later advanced airway management and causes an increase in the risk of death from pneumonia in the ICU setting if initial resuscitation is successful [21].
3. After the first shock is delivered, the majority of firefighters reported pausing compressions for a pulse check. It is important to resume post-shock compressions immediately after the shock due to the fact that most individuals are converted to a non-perfusing rhythm – the mean interval of asystole following defibrillation for patients that regain a pulse is 77 seconds [22]. Prehospital care providers cannot stand idly by during this period, and must continue acting as a surrogate for the patient’s heart to minimize the damage to their brain and other organs.
Once these steps (200 pre-shock compressions coupled with AED pad placement and initiation of passive oxygenation, rapid defibrillation, and 200 post-shock compressions) are followed, the compression and defibrillation steps can be repeated until EMS arrives on scene and care can be transferred. Using these methods, the chances of obtaining return of spontaneous circulation during the initial phase of management by first responders will be multiplied. This early resuscitation success has the potential to produce an increased number of neurologically intact survivors – the gold standard outcome and holy grail for every prehospital provider.
Focusing on improving the knowledge and BLS resuscitation skills of volunteer fire department members has the potential to revolutionize the standard of care for this critically ill class of patients in my agency’s service area and in communities across the country that find themselves in a similar situation. Proper implementation entails concerted outreach by EMS agencies to the members of volunteer fire departments to ensure that they are trained in the proper management methods and possess the required equipment to properly resuscitate victims of sudden cardiac arrest in an evidence-based manner. It is the duty of prehospital care providers who are trained in resuscitation and have a familiarity with the underlying physiological reasons for the cutting-edge methods we employ in the field to take this knowledge and put it in the hands of people who can use it to save lives.
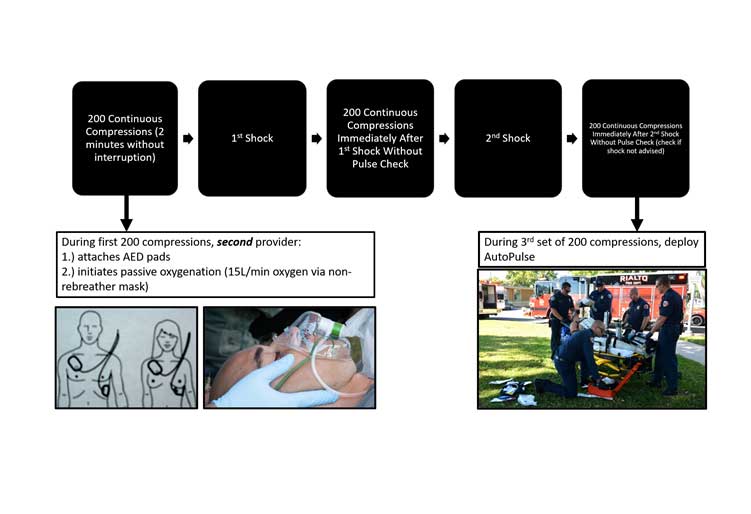
At this time, I am focusing my efforts on providing interactive, lecture-based instruction to the fire departments within our EMS agency’s service area. In addition to this large-group format, it may be beneficial to institute repeat training sessions at regular intervals following this initial introduction (i.e. mandatory quarterly review of an instructional video detailing the “how” and “why” of the methods being employed). To facilitate adherence to the protocol in addition to decreasing the cognitive load of providers while they are engaged in an activity as stressful as resuscitation. I have prepared a graphic representation of the protocol (Figure 1) that is included in the medical bags and clipboards carried by fire department vehicles. On the back of each of these protocol sheets, I also included a QA questionnaire and checklist that all first responders have been instructed to complete immediately after clearing the scene of an arrest. Inclusion of the required completion this checklist also serves to reinforce the correct methodology to providers.
The goal of this document is to present a convincing case to EMS administrators and providers that volunteer first responders have a significant, often underutilized value to the practice of resuscitation in communities that experience EMS response times to cardiac arrests that exceed four minutes. In addition, I hope that this writing will serve as a blueprint to enact change and facilitate the construction of improved systems of care for arrest victims in rural and semi-rural communities. In the end, it all comes down to one fact. No matter how good you are at providing prehospital care as an AEMT, paramedic or prehospital physician, the war to save a victim of sudden cardiac arrest is already lost if invasive, purposeful intervention is not initiated within minutes of pulselessness. To save lives, it’s paramount that we educate first responders about the proper performance of CCR.
Tanner Smida is a student cardiac arrest resuscitation researcher with the University of Pittsburgh Department of Emergency Medicine. On the weekends, he serves the communities of Monessen, Charleroi, and Donora, Pennsylvania as an employee of Mon Valley EMS.
REFERENCES
1. Larsen, M.P., et al., Predicting survival from out-of-hospital cardiac arrest: a graphic model. Ann Emerg Med, 1993. 22(11): p. 1652-8.
2. Hallstrom, A.P., et al., Public-access defibrillation and survival after out-of-hospital cardiac arrest. N Engl J Med, 2004. 351(7): p. 637-46.
3. Kitamura, T., et al., Nationwide public-access defibrillation in Japan. N Engl J Med, 2010. 362(11): p. 994-1004.
4. Ringh, M., et al., Survival after Public Access Defibrillation in Stockholm, Sweden–A striking success. Resuscitation, 2015. 91: p. 1-7.
5. Nichol, G., et al., Regional variation in out-of-hospital cardiac arrest incidence and outcome. JAMA, 2008. 300(12): p. 1423-31.
6. Kellum, M.J., et al., Cardiocerebral resuscitation improves neurologically intact survival of patients with out-of-hospital cardiac arrest. Ann Emerg Med, 2008. 52(3): p. 244-52.
7. Ewy, G.A., Cardiocerebral and cardiopulmonary resuscitation – 2017 update. Acute Med Surg, 2017. 4(3): p. 227-234.
8. Salmen, M., G.A. Ewy, and C. Sasson, Use of cardiocerebral resuscitation or AHA/ERC 2005 Guidelines is associated with improved survival from out-of-hospital cardiac arrest: a systematic review and meta-analysis. BMJ Open, 2012. 2(5).
9. Ewy, G.A., Do modifications of the American Heart Association guidelines improve survival of patients with out-of-hospital cardiac arrest? Circulation, 2009. 119(19): p. 2542-4.
10. Garza, A.G., et al., Improved patient survival using a modified resuscitation protocol for out-of-hospital cardiac arrest. Circulation, 2009. 119(19): p. 2597-605.
11. Bobrow, B.J., et al., Minimally interrupted cardiac resuscitation by emergency medical services for out-of-hospital cardiac arrest. JAMA, 2008. 299(10): p. 1158-65.
12. Berg, R.A., et al., Magnetic resonance imaging during untreated ventricular fibrillation reveals prompt right ventricular overdistention without left ventricular volume loss. Circulation, 2005. 111(9): p. 1136-40.
13. Steen, S., et al., The critical importance of minimal delay between chest compressions and subsequent defibrillation: a haemodynamic explanation. Resuscitation, 2003. 58(3): p. 249-58.
14. Valenzuela, T.D., et al., Interruptions of chest compressions during emergency medical systems resuscitation. Circulation, 2005. 112(9): p. 1259-65.
15. Niemann, J.T., et al., Treatment of prolonged ventricular fibrillation. Immediate countershock versus high-dose epinephrine and CPR preceding countershock. Circulation, 1992. 85(1): p. 281-7.
16. Berg, R.A., et al., Precountershock cardiopulmonary resuscitation improves ventricular fibrillation median frequency and myocardial readiness for successful defibrillation from prolonged ventricular fibrillation: a randomized, controlled swine study. Ann Emerg Med, 2002. 40(6): p. 563-70.
17. Cobb, L.A., et al., Influence of cardiopulmonary resuscitation prior to defibrillation in patients with out-of-hospital ventricular fibrillation. JAMA, 1999. 281(13): p. 1182-8.
18. Wik, L., et al., Delaying defibrillation to give basic cardiopulmonary resuscitation to patients with out-of-hospital ventricular fibrillation: a randomized trial. JAMA, 2003. 289(11): p. 1389-95.
19. Berg, R.A., et al., Adverse hemodynamic effects of interrupting chest compressions for rescue breathing during cardiopulmonary resuscitation for ventricular fibrillation cardiac arrest. Circulation, 2001. 104(20): p. 2465-70.
20. Aufderheide, T.P., et al., Hyperventilation-induced hypotension during cardiopulmonary resuscitation. Circulation, 2004. 109(16): p. 1960-5.
21. Simons, R.W., et al., The incidence and significance of emesis associated with out-of-hospital cardiac arrest. Resuscitation, 2007. 74(3): p. 427-31.
22. Pierce, A.E., et al., The need to resume chest compressions immediately after defibrillation attempts: an analysis of post-shock rhythms and duration of pulselessness following out-of-hospital cardiac arrest. Resuscitation, 2015. 89: p. 162-8.
The author would like to thank David Salcido, MPH, PHD, Leonard Weiss, MD, and Donora Volunteer Fire Company Captain Donny Foster for critically editing the manuscript. In addition, he would like to thank the members of the Charleroi VFD, Fallowfield Township VFD, Donora Volunteer Fire Company, and Mon Valley EMS for their heroic efforts to resuscitate cardiac arrest victims.

