
fireEMS ❘ By Nick Paproski
You are dispatched to a baby reported not to be breathing. While you are en route, dispatch updates you that the baby is now alert and crying. You arrive to find the parents frightened and the baby alert and breathing normally, with no obvious distress. The mother explains that during feeding, the baby suddenly stopped breathing for a few seconds, turned pale, and became very rigid. Within less than a minute, the baby started to cough and cry. What should be your plan of action? Is transport necessary?
What was ALTE?
Prior to the term “Apparent Life Threatening Event” (ALTE), occurrences like this case were frequently referred to as “near-miss Sudden Infant Death Syndrome (SIDS)” or “aborted crib death.”1 An already stressful experience was made infinitely worse when parents were (incorrectly) told that their child was now at an increased risk of SIDS. After many years, the belief that SIDS was somehow connected with ALTE was found not to be true.
RELATED
Engine Company EMS: Pediatric Patients
Pediatric Seizures: Routine or Danger in Disguise?
In 1986, the National Institutes of Health Consensus Panel on Infantile Apnea and Home Monitoring coined the term “ALTE” in an attempt to classify and better study an emerging phenomenon. ALTE describes “a frightening constellation of symptoms in which the child exhibits some combination of apnea, change in color, change in muscle tone, coughing, or gagging.”1 Unfortunately, this definition had several limitations. Primarily, the term “life threatening” was left to the subjective opinion of a family member when, in reality, what a family member may have deemed life-threatening could easily have been a benign event. Additionally, there was very little evidence-based guidance to assist health care providers in formulating a care plan once ALTE was suspected.
Acknowledging the limited guidance available, medical directors often advised emergency medical services (EMS) providers to tell family members that ALTE could be a warning sign for more serious problems.2 The goal was to have EMS cast a large net by intentionally overtriaging. Following transport, emergency department physicians were tasked with the job of figuring out how to work up these patients. In hospitals, infants were frequently subjected to a battery of invasive tests and sometimes even hospital admissions. Testing ultimately had very low yields and tended to be performed with a high degree of variability from provider to provider.3
With these difficulties in mind, the American Academy of Pediatrics (AAP), in 2013, convened a subcommittee to study the available ALTE literature with the goal of developing a clinical practice guideline (CPG).4 In 2016, the AAP approved the committee’s CPG. While initially perceived as merely a name change, the CPG recommendations represented a significant shift in our understanding about these phenomena. It also provided prehospital professionals with a detailed framework for assessment and treatment of infants who experience these short, scary, and unexplained events.

(1) Respiratory distress alone does not make an event a BRUE. BRUE criteria identified significantly decreased, irregular, or no breathing. (Photos by Rommie Duckworth.)
What Is a BRUE?
The first recommendation of the AAP CPG was to replace the term “ALTE” with “Brief Resolved Unexplained Event” (BRUE). BRUE (pronounced “brew”) means exactly what the name suggests—“an event occurring in an infant younger than 1 year when the observer reports a sudden, brief, and now resolved episode of ≥ 1 of the following: (1) cyanosis or pallor; (2) absent, decreased, or irregular breathing; (3) marked change in tone (hyper- or hypotonia); and (4) altered level of responsiveness”4 (Figure 1).
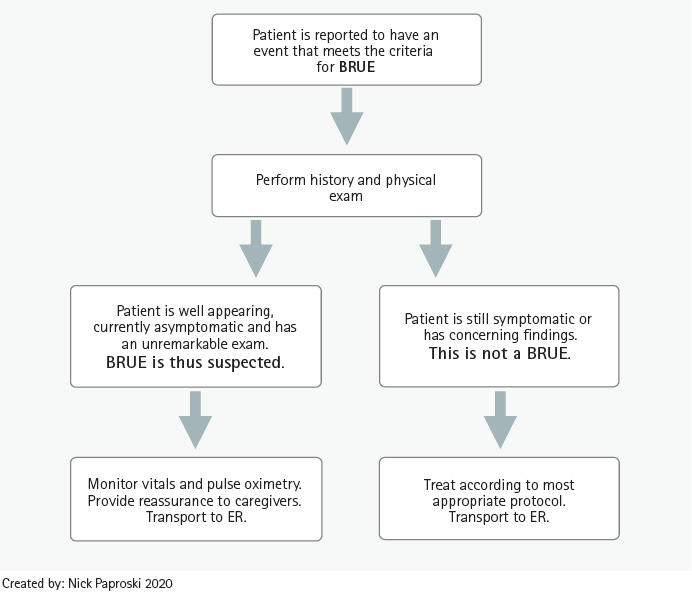
Figure 1. Prehospital BRUE Identification and Treatment
- Cyanosis: To meet the criteria for BRUE, the cyanosis observed must be central cyanosis. Blue nail beds in the absence of other symptoms is a common or normal physical finding for an infant that is often associated with their hands being cold, especially in neonates.3 It is also common to observe changes in skin color during a coughing or choking episode. It is important that providers have a solid understanding of what is normal for an infant.
- Absent, decreased, or irregular breathing: Respiratory distress alone does not meet the criteria for BRUE. The definition requires there be no breathing or significantly decreased or irregular breathing.
- Change in tone: Implies being either completely limp or rigid.
- Altered level of responsiveness: The infant could be described as being lethargic, difficult to wake up, or completely unresponsive.
A history frequently heard from parents is that the child was found in the crib initially unresponsive, with limp muscles, and there were questions as to whether or not the baby was breathing. The child starts breathing normally and becomes active when picked up. All of this occurs within less than one minute. By the time EMS arrives, the infant is completely back to his baseline and has a normal exam. Such a case would meet the definition of BRUE because it lasted less than one minute, resolved completely, and has no immediate or obvious explanation.

(2) The American Academy of Pediatrics has published recommendations for how EMTs and paramedics can best deal with these brief, frightening events.
What Is Not a BRUE?
If the infant has not returned to his baseline at the time of EMS’ arrival, it was not a BRUE. Persisting symptoms such as a cough, fever, or an altered level of consciousness should be investigated and the pathologies treated according to protocol and best practices.
Any event that has an obvious or a likely cause also excludes it from being considered a BRUE. For example, an infant that has a coughing spell and a period of color change during a feeding previously would have met the criteria for ALTE but would have been considered a BRUE. This is a good example of how the more specific definition excluded many of the cases that would have been included under the overly broad definition of ALTE.
Which Infants Are at High Risk?
If the infant is less than 60 days old and has had multiple events and if the event lasted longer than a minute or CPR [cardiopulmonary resuscitation] was administered, the baby should be considered to be in a high-risk category.4 Infants with high-risk criteria have an increased risk of recurrence of events or eventual adverse outcomes. IVs should only be placed when a provider has clinical concerns for shock or if intravenous medications are necessary. IVs should not be routinely started on infants who have a BRUE.5 Although infants in this high-risk group may be asymptomatic at the time of the EMS providers’ exam, they should be monitored closely and transported to a facility with pediatric critical care capability.5
What About Low-Risk Infants?
The AAP subcommittee identified a subset of BRUE patients who are “unlikely to have a recurrent event or undiagnosed serious condition, [and] are at a lower risk of adverse outcomes.”4 A low-risk infant with a BRUE is one who doesn’t meet any of the high-risk criteria (is older than 60 days, has only had a single event, and did not receive CPR).
During transport, the patient should be observed continuously for changes in condition and recurrence of symptoms. Continuous pulse oximetry should be utilized.5 A cardiac monitor may be applied5; however, the CPG notes that there is weak evidence to support the utility of routinely obtaining a 12-lead EKG.4
These low-risk patients will likely require only a short period of noninvasive monitoring in the emergency department (ED). Although the length of time required for monitoring has not been well studied, the CPG recommends ED monitoring for 1-2 hours.3 Knowing this can be of significant reassurance to parents who, when you mention the idea of transport to the ED, may be envisioning their infant undergoing spinal taps and endoscopies. Transport for low-risk BRUE patients should be explained to parents as a highly precautionary measure.
What Should Providers Do?
If providers identify that the patient has had a BRUE, the first step should be to perform a detailed history and physical exam, including a full set of vital signs. The results are essential for excluding differential diagnoses such as fever, hypoglycemia, trauma, child abuse, and seizures. BRUE is ultimately a constellation of symptoms, not a disease process5; its diagnosis rests on being able to successfully rule out differential diagnoses. Completing a detailed physical and history allows providers to identify finding any signs or vitals that would point to an underlying condition being responsible for the observed symptoms.
Once a provider is confident that the patient has experienced a BRUE, the next step is to reassure the patient’s caregivers. They should be told that a detailed exam and history have not produced any abnormal findings. Providers should feel comfortable explaining to parents that they are treating the patient as if they have had a BRUE and explaining what a BRUE is (See “What is BRUE?”). They should explain that the treatment plan for all BRUE patients is to provide noninvasive monitoring on the way to the hospital where the infant will be evaluated again by a physician.
Should the parents wish to sign a refusal, consult online medical direction, especially if the patient meets high-risk criteria.5 While the relative risk to patients considered low risk is now better understood,4 there is not yet enough data to support the safety of routinely obtaining refusals in this population. Ultimately, the most practical way for these patients to receive the recommended period of monitoring is to transport them to the ED.
What Is a BRUE?
Brief. The event lasted less than one minute.
Resolved. The symptoms have completely resolved upon arrival of EMS.
Unexplained. The event is not attributable to any other occurrence such as choking, fever, or a seizure.
Event. BRUE is not a disease; it is a group of symptoms. There is no diagnostic test that can identify when a patient has had one. Diagnosis is made by ruling out differentials.
Source: NASEMSO Scope of Practice, 2018.
In line with an AAP policy statement on CPR, the CPG also recommends that the infant’s caregivers be offered CPR training. Bystander CPR is associated with improved one-month outcomes in pediatric patients following an out-of-hospital cardiac arrest. CPR training has not been shown to increase caregiver anxiety and, in fact, caregivers have reported a sense of empowerment.4 EMS providers should be aware of local or department CPR training resources so they can make appropriate referrals to caregivers.3
Is BRUE related to SIDS?
At this point, there is no identifiable correlation between ALTE and BRUE and SIDS.4 The incidence of SIDS is similar in infants who have had a BRUE when compared to those who haven’t. Additionally, initiatives believed responsible for reducing SIDS incidences (such as the Back to Sleep campaign) have had no impact on the incidence of BRUE.1 SIDS and BRUE have very different sets of risk factors.3 For these reasons, EMS providers should refrain from telling caregivers that BRUE is a risk factor for SIDS.
The Future for BRUE
What can EMS professionals do to facilitate research on this topic? The most important contribution would be to use the term BRUE in documentation. With the majority of services using ePCR software, a growing body of data can be mined for research. The NEMSIS terminology has yet to reflect the new terminology, but the older ALTE term can be used until this occurs.5
The AAP BRUE subcommittee plans to release more specific guidance for the management of high-risk BRUE patients in the future.3 With a more precise definition available, data collection and follow-up of these cases can be enhanced. Additionally, prehospital protocol committees should look to integrate the insights from the CPG into protocols. The National Model EMS Guidelines are an excellent, up-to-date resource for drafting EMS protocols.
A thorough history and physical exam comprise the cornerstone for identifying underlying pathologies that would rule out a diagnosis of BRUE. If a BRUE is suspected, providers should feel confident in their understanding of the relative risks these patients face. Patients should be transported to the most appropriate facility and monitored continuously during transport. In these cases, providers have the profound opportunity to treat the patient and caregivers in a professional, calm, and reassuring manner. This can well serve to reduce the inevitable anxiety provoked by an event that parents may remember as one of the scariest of their lives.
References
1. Hall, KL & Zalman, B. (2005, June 15). Evaluation and Management of Apparent Life-Threatening Events in Children. Retrieved January 12, 2019, from https://www.aafp.org/afp/2005/0615/p2301.html.
2. Maggiore, WA. (2014 December 4). Assessing Apparent Life-Threatening Events in Infants. Retrieved from https://www.jems.com/2014/12/04/assessing-apparent-life-threatening-even/.
3. Brief Resolved Unexplained Events. (2017) Retrieved from https://www.youtube.com/watch?v=mMGgBEcVQUs/.
4. Tieder, JS. (2016 May). Brief Resolved Unexplained Events (Formerly Apparent Life-Threatening Events) and Evaluation of Lower-Risk Infants. Retrieved January 2019, from https://pediatrics.aappublications.org/content/137/5/e20160590.
5. NASEMSO Scope of Practice 2018; https://www.ems.gov/pdf/advancing-ems-systems/Provider-Resources/National-Model-EMS-Clinical-Guidelines-September-2017.pdf.
NICK PAPROSKI is an award-winning paramedic field provider and educator. He began his EMS career as an EMT with Newtown (CT) Volunteer Ambulance in 2005. He has served as a career paramedic/firefighter with the Ridgefield (CT) Fire Department since 2010 and as the chief safety officer for Vintech Management Services in Torrington, Connecticut, since 2018. He is an adjunct instructor with the New England Center for Rescue and Emergency Medicine. He has presented on the topic of BRUE at the March 2020 EMS Today conference.

