
By Todd LeDuc and Dr. Sara Jahnke
The United States has been impacted by a global pandemic that, as of this writing, has claimed nearly 54,000 American lives. Of those deaths, 88 were reported to be first responders and 27 have been health care workers. The Centers for Disease Control and Prevention (CDC) further estimates that health care workers account for 11 percent of all COVID-19 infections, which as of this writing stand at 958,863. The International Association of Fire Chief’s (IAFC) COVID-19 Web site reports that 12,737 fire service personnel have been exposed to the virus; 12, 455 reported to be quarantined and 685 have been diagnosed with the virus. Given this information is self-reported, it is likely a vast underrepresentation of the magnitude of impact on first responders. The International Association of Fire Fighters (IAFF) has reported that 1,653 of their members have tested positive for COVID-19, with 66 being hospitalized and six deceased.
Reports of hospitalizations and deaths from COVID-19 seem to be strongly correlated with age and other co-morbid underlying medical conditions such as hypertension, cardiac, diabetes, obesity, and pre-existing respiratory conditions as well as advanced age.
The literature has reported that first responders may have higher rates of these co-morbid conditions, such as excess weight/obesity often associated with metabolic syndrome and elevated blood glucose and lipid levels, hypertension, and cardiovascular risk. These increased rates are likely the result of a number of occupational exposures as outlined in recent research. Additionally, first responders have repeated exposures to the coronavirus because of the nature of their job.
To date, most reported public health and research efforts are focusing on stemming the spread, “flattening the curve,” testing capabilities, therapeutic treatment modalities, and vaccines to promote immunity. Little has been reported on studying the potential long-term health consequences, particularly to first responders and health care providers who were exposed, infected, and likely re-exposed. This is perhaps an even more pressing question to examine given these first responders have a well-documented elevated rate of occupational health risks including excess weight, cardiovascular, cancer, and challenges to immune systems in the form compromised sleep, behavioral health risks, and nutritional challenges and the negative effects of shift work.
After September 11, 2001, a concern emerged of long-term health consequences for those impacted at “Ground Zero” after the attacks on the World Trade Center. In 2010, the “World Trade Center Health Program” was established. The James Zadroga 9/11 Health & Compensation Act—named for a New York City police officer whose death was linked to his work at Ground Zero—helps people with illnesses that have a documented link to the disaster. Dr. Michael Crane, who directs the program at the Icahn School of Medicine at Mount Sinai Hospital in New York, says 72,000 people are enrolled, including firefighters and police officers but also utility workers, medical examiners, and others. Of them, he says 8,000 already have cancer.
Prior work published by the IAFC has demonstrated that 20 percent of career firefighters and as much as 40 percent of volunteer firefighters receive no annual occupational medical exam and many more receive an exam not aligned with the occupational health risks of firefighting. Additionally, National Fire Protection Association 1582, Standard on Comprehensive Occupational Medical Program for Fire Departments, was not designed nor intended to address long-term health monitoring of a viral pandemic exposure and the effects on first responders. These health effects certain will be presumed to include behavioral health and wellness challenges and disorders from the repeated traumatic exposures, such as in the case of a leading emergency medicine doctor in New York City who had contracted the virus and subsequently committed suicide, reportedly from the overwhelming toll of the influx of COVID deaths. While there has been reported debate of recent as to whether COVID-19 should be entitled to receive line-of-duty death (LODD) benefits, it appears many are being treated as LODDs.
We would suggest that the time for a national discussion about a first responder and health care provider medical monitoring system is now rather than years from now when unseen health consequences finally may be recognized. This can be couched in scientific design or afford greater access to proper occupational medical surveillance.
While questions and design of a long-term surveillance system are in discussion, it is imperative that firefighters be encouraged to track their exposures to the virus. Several tracking programs exist both specific to the virus and also for exposures in general. For instance, the National Fire Operations Reporting System exposure tracking system has questions specific to calls suspected or known to be COVID-19 exposures. Questions include details about practices and personal protective equipment. The tracking program is available for free to any firefighter who wants to track their own work. These can some day be integrated with other surveillance measures to monitor the long-term impacts to the first responder community.
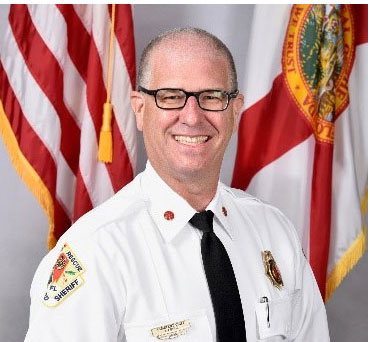
Todd J. LeDuc, MS, CFO, FIFirE, retired after nearly 30 years as assistant fire chief of Broward County, Florida, an internationally accredited career metro department. He served as chief strategy officer for Life Scan Wellness Centers, a national provider of comprehensive physicals and early detection exams. He has served as a member of the International Association of Fire Chief’s Safety, Health & Survival Section for over a decade and is currently secretary of the section. He is a peer reviewer for both professional credentialing and agency accreditation. He is editor of Surviving the Fire Service (Fire Engineering Books) and serves on numerous advisory boards and publications. He can be contacted at Todd. LeDuc@lifescanwellness.com
Sara A. Jahnke, Ph.D. is the director of the Center for Fire, Rescue and EMS Health Research at the National Development and Research Institutes. She was the principal investigator on two large-scale, DHS-funded studies of the health and readiness of the U.S. fire service and on a study on the health of women firefighters. She is a co-investigator of several studies focused on fitness, nutrition and health behaviors in firefighters. She completed her doctorate in psychology with a health emphasis at the University of Missouri – Kansas City and the American Heart Associations’ Fellowship on the Epidemiology and Prevention of Cardiovascular Disease.
This commentary reflects the opinion of the author and does not necessarily reflect the opinions of Fire Engineering. It has not undergone Fire Engineering‘s peer-review process.

