
By Christopher L. McKenna
Few would dispute that being a firefighter or an emergency medical technician (EMT) is a dangerous and a stressful occupation. Despite the risks, 1.13 million men and women served in the fire service in 2014, of which nearly 69 percent served on a voluntary basis.1 Moreover, these individuals responded to approximately 31.6 million calls across the country in 2014, ranging from fires to requests for medical aid, hazardous materials, and false alarms.2 Undoubtedly, many of these situations result in exposure to traumatic or stressful situations. Not surprisingly, those in the fire service have higher rates of depression and suicide.3 This raises the question of whether these bold individuals are getting the help they need to combat the, at times, difficult encounters.
For example, a recent study showed that 58 percent of almost 500 participants were more likely to report stigma-related barriers to care as members of the fire service.4 For decades, the fire service has convinced members that they are superheroes and that nothing can get to them. In recent years, however, the spotlight has illuminated the alarming suicide rate in the fire service. Some authors believe that the effects of this stigma cause individuals not to seek mental health care for fear of being labeled as weak or as unfit for duty. (4)
Unfortunately, research on the stigma associated with mental health services among members of the fire service has been overlooked in the existing literature. As such, this article looks at how the stigma affects firefighters in their daily lives and the struggles they face while attempting to seek treatment. Some of the recent firefighter suicide studies point out that one of the reasons the suicide rate might be so high is that firefighters do not seek mental health treatment.5 Arguably, firefighters avoid help as a result of the stigma attached to mental health care in the fire service. This stigma labels anyone who seeks mental health treatment as weak and not a real firefighter because they are unable to handle the stresses of the job. The stigma was created by members of the fire service because some truly believe they are superheroes and nothing can hurt them. Yet, not seeking mental health treatment when it is needed can potentially have some drastic effects on a person’s life. On October 15, 2016, Indian River County, Vero Beach, Florida, Fire Rescue Battalion Chief David Dangerfield committed suicide after posting the following to his Facebook page:
“PTSD [post-traumatic stress disorder] for Firefighters is real. If your loved one is experiencing signs, get them help quickly. 27 years of deaths and babies dying in your hands is a memory that you will never get rid of. It haunted me daily until now. My love to my crews. Be safe, take care. I love you all.”6
David’s father, Bruce Dangerfield, confirmed that “[David] was seeing a doctor for a year and a half, about three days a week, to deal with PTSD.”7 The fact that it took Chief Dangerfield more than 25 years to seek mental health treatment is upsetting. Could his death have been avoided if he had felt comfortable seeking treatment sooner? We will never know, but we can work to change this stigma against mental health in hopes of saving someone else’s life.
Firefighters’ Perspectives
Recently, as I have discussed this research with friends, people have reacted in one of two ways. Some view this research as a great topic that has the potential to produce very eye-opening results. Others respond by saying, “Why would someone waste so much time and effort to research such a worthless topic?” These perspectives represent the current rift within the fire service pertaining to mental health services. My goal is not to quantify how many members of the fire service ascribe to these two perspectives. The primary objective is to examine the extent to which this stigma is real among a group of fire service personnel and the perceived consequences associated with it.
Members of the fire service (firefighters, EMTs, and paramedics) risk their lives daily for people they have never met. The traumatic sights to which they are exposed would make a normal person cringe. Firefighters/EMTs have to remain calm and focused while treating those seriously injured while trying to suppress what they are seeing. Yet, once an incident is over, the experience begins to set in. Some try to brush it off, saying, “It is just another day in my life.” Some are so affected that it changes their life drastically. For example, some might finally realize that they need to seek help to be able to sleep through the night to avoid reliving the incident. However, when they are treated differently by their peers because they seek help, the problem becomes immensely harder to deal with.
We cannot expect the people who risk their lives for strangers to just shrug off the horrible images they see and go about life as if nothing happened. Mental health requires support, not the division created by this stigma. Left untreated, PTSD can lead to unthinkable consequences. Although not everyone exposed to serious incidents gets PTSD, some do; and those people need support to overcome the worst of it and begin to heal.
The fire service exists to help people in need. Why can’t it help its own members? Yes, the sights that fire service personnel see are horrific, but there needs to be support for those who need help to process these experiences. Departments need to confront this stigma head-on; moreover, they should encourage their members to seek mental health care to divert any potential mental issues later in life. If we do not take care of our firefighters, EMTs, and paramedics when they are in need, who will take care of us when we are in need?
Stigma Evident in Military as Well
Suicide in the fire service is growing at an alarming rate.8 It was only in 2010 that Captain (Ret.) Jeff Dill decided to undertake the task of tracking firefighter suicides in the United States.9 According to the Firefighter Behavioral Health Alliance Web site, the number of firefighter suicides in the United States was 81 in 2012; 70 in 2013; 112 in 2014; 132 in 2015; and 111 in 2016, the last figures reported. We should not look at firefighter suicides in the United States only. Dill began to look at international firefighter suicides in 2013. The fact is that the fire service has a growing rate of suicide for two main reasons: a cultural stigma against mental health care and untreated mental health disorders.10
In trying to understand why firefighter suicide is on the rise, a recent report found that 58 percent of 483 firefighters in the study “reported stigma-related barriers to care.” (4) In the same study of those 483 firefighters, [t]he most frequently cited stigma-related barriers were concerns about being treated differently by peers (44%, N=210), appearing weak (42%, N=205), having a harmed reputation (41%, N=198), being thought less of by others (37%, N=178), embarrassment (30%, N=147), and being blamed (26%, N=126). (4)
This study shows that fear of fire service members to seek mental health services is a factor in the high suicide rate. The stigma against mental health is not limited to the fire service. This stigma has for years lived in the ranks of the United States military. In a study conducted on soldiers returning from Iraq, those who had scored positively for mental health problems (in an interview required of all soldiers prior to returning home) were twice as likely to report fear of stigmatization and concern about barriers to obtaining mental health treatment.11
The authors of this same report found it crucial to understand what the meaning of a stigma is and to define the two types of stigma faced by returning military personnel. Stigma is defined as “a negative and erroneous attitude about a person; it is a prejudice or negative stereotype.” (11) There are two types of stigma: public stigma and self-stigma. “Public stigma is the reaction of the general public toward people with mental illness; self-stigma is the internalization of how the general public portrays people with mental illness and the belief in that portrayal.” Although these types of stigma are distantly different, they are composed of stereotypes and discrimination. (11) The stigma attached to mental health treatment may damage a person’s self-esteem and hinder treatment needed.12
In the military, it is harder for soldiers to report potential mental health problems than medical problems. (11) Soldiers deployed to Afghanistan and Iraq reported feeling that if they asked for mental health services, they would feel embarrassed and appear as weak. (12) In a study that compared active duty military to National Guard soldiers, it was found that “active duty soldiers consistently reported higher perceptions of stigma than National Guard soldiers at three and 12 months postdeployment … active duty respondents endorsed stigma twice as often as their National Guard counterparts.”13
The need for mental health treatment in both the military and the fire service starts with the exposure to a traumatic event. In the military, 90 percent of soldiers returning from war have been exposed to a traumatic event. (11) There is no way to measure how many fire service personnel are exposed to a traumatic event during their time in the fire service, but one can speculate it is nearly every member of the fire service. If soldiers or firefighters internalize the stigma behaviors of those around them, they are likely to develop a self-stigma. (11)
“The development of a self-stigma has been hypothesized to lower one’s self-esteem, which, in turn, could inhibit one’s ambition to seek mental health care.” (11) On some occasions, individuals may view themselves as responsible for their disorder because they feel they should have control over their mind or they may feel responsible for experiencing symptoms of PTSD. (11) A better understanding of these stigmas will help individuals to see why soldiers and firefighters would choose to avoid seeking mental health treatment. This stigma against mental health is affecting professions in which people serve others; the fire service and the military are just two examples.
Members of the fire service and the military have voiced concerns about their reputation and being embarrassed. (4) Both express a need to decrease this stigma to increase treatment for their members. (11, 4) In his article, “The Stigma of Mental Health Problems in the Military,” Thomas W. Britt refers to a three-method program aimed at reducing the stigma attached to mental illness. The first strategy is protesting, an attempt to suppress the stigmatizing attitudes and behaviors. This would serve to inform society that it should not hold negative stereotypes or prejudices against mental illness. The second strategy is educating society on mental disorders. This is meant to provide realistic descriptions of problems, including the cause of the problems and how different problems can be addressed through a variety of treatments. The third strategy is to promote contact with individuals who have a mental illness. This is aimed at showing others that having a mental illness does not turn one into a bad person. This was the option that most successfully reduced the stigma. (11)
The fire service has also found a successful method for reducing this stigma. A study found that a two-day training program on mental health awareness and promoting the use of counselors was helpful to management in departments and even changed many chiefs’ attitudes toward mental health programs.14 In addition, the National Fallen Firefighters Foundation (NFFF) started a program called “Everyone Goes Home,” which is focused on “16 Life Safety Initiatives” designed to give the fire service a blueprint for making changes.15 The 13th initiative advocates psychological support for firefighters and their families.
Challenges to Treating Firefighters
Mental health providers face challenges when treating firefighters. The main problem is the stigma against seeking help, which often causes fire service members to distrust the mental health professionals. To prepare for this distrust, “it is imperative that clinicians who wish to work in this area have an in-depth knowledge of firefighter culture.” (10) Funding is another challenge for department and health professionals who want to work with first responders. “Large departments often have greater funding to provide a multitude of resources, which leaves a substantial gap of resources for a majority of the fire service, which operates on volunteers.” (10) Volunteer departments are unable to afford a number of resources large departments provide their members. As a result, volunteer departments are often overlooked. Most departments that do not have a program already established should have mental health professionals assist them in establishing policies and procedures to address suicide and mental health. (10)
Houston Fire Department Program
The Houston (TX) Fire Department (HFD) has implemented a successful Suicide Prevention Program. The impetus for the program was three active duty suicides and four retiree suicides that occurred between 2001 and 2007. The department’s administration worked with Baylor College of Medicine and the HFD Physiological Services to create a peer-based suicide prevention program.
The team consisted of nine active duty firefighters who received basic training on suicide and mental health. The program was well received and the team members received additional training and functioned as an internal unit working alongside the staff psychologist and other team members. Since the program was implemented in 2007, there have been no suicides within the department. (10) Peer-based and other in-house programs are essential in tackling the stigma toward mental health. (10)
“The stigma associated with mental illness, and especially suicide, is one reason people are reluctant, even as gatekeepers, to get involved or intervene.”16 The suicide rate in the fire service is climbing at an alarming rate, and the stigma is contributing to the climb. Members of the fire service are not invincible when it comes to experiencing PTSD symptoms. If the fire service does not come together to destroy this stigma, the fire service will slowly destroy itself. This research is meant to be that starting place for the fire service. In raising awareness of this issue, my objective is to start that discussion about the stigma and what we can do to create a friendly environment toward mental health in the fire service. Becoming proactive to attack this stigma is the only way to save future lives that may be lost to suicide.
Social Theory
Social theory plays an enormous role in the struggle with mental health stigma. A theory that can help explain this issue is “labeling theory,” which was created in the early 1960s.17 A simple definition of the labeling theory is that “societal reaction in the form of labeling or official typing, and consequent stigmatization, leads to an altered identity in the actor, necessitating a reconstitution of self.” (17) In other words, this theory explains how the self-identity and behavior of individuals can be determined or influenced by the way others describe them. The theory is based on the concept that people accept as their personal identity a label given to them by others—others see them as weak, and they come to look on themselves as weak.
Being labeled in the fire service creates barriers between the individuals and their fellow firefighters. So often people think of the fire service as a tightly knit family that is always there for each another. That is not always true. When people finally build up the courage to admit they need help and ask for it, sometimes that family leaves them. With the stigma that exists in the fire service, when someone asks for help, he runs the risk of being labeled as weak or unfit for the job by members who were once considered “family.” The person asking for help loses a great deal of support through this process.
Labeling someone unfit or weak because of a request for mental health care after witnessing what first responders see daily creates an environment in which self-care is viewed as insignificant. No one should be labeled because they need to process what they have seen, nor should they have to contend with any push-back from their peers.
Study: Consequences of Mental Health Stigma
The primary objective of this project was to assess the existence and perceived consequences of the mental health stigma in the fire service. The method used was firsthand accounts obtained through interviews. The project was approved by the Mount St. Mary’s University Institutional Review Board in October 2016.
Participants and Procedures
Volunteers were recruited through flyers posted at the National Fire Academy and fire stations around the greater Washington, D.C., area. The participants volunteered for the project and chose the place of the interview, which was conducted in a semi-structured format. The individuals were asked a set of questions; if additional questions presented themselves during the interview, they were asked as well. The study focused on eight members of the fire service (N=8), unfortunately falling short of the original goal of 15 participants.
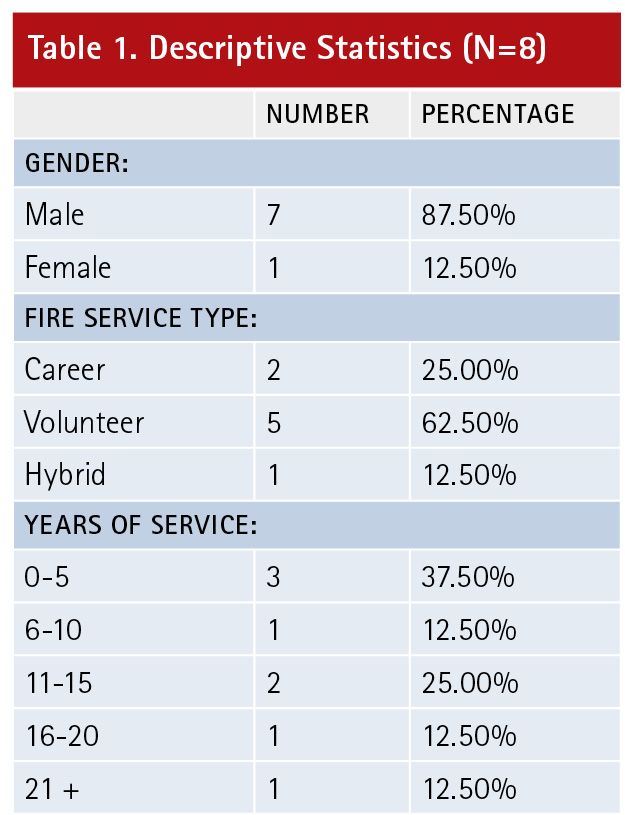
The participants came from a variety of backgrounds in the fire service. For this study, the term “fire service” includes career, volunteer, and “hybrid” (both career and volunteer) firefighters. (5) Participants consisted of five volunteers, two career firefighters, and one hybrid firefighter; seven were male and one was female. The percentage of male to females in this study was slightly lower than the national percentage of the fire service. As of 2014, the fire service (both career and volunteer) was comprised of 1.051 million males and 82,550 females.18 Flyers for this project were posted from mid-October 2016 through the end of January 2017. A second “posting” of the flyer was done around the end of November in hopes of attracting more interest. Interviews were electronically recorded and then stored on an encrypted hard drive. The audio files were transcribed to enable further analysis.
Analytical Strategy
Content analysis (the “systematic analysis of the symbolic content of communications in which the content is reduced to a set of coded variables or categories”19) was used to examine and study the interviews. Within my research, I analyzed the transcripts of the interviews and coded them into categories based on what I considered the most important information to include in the final report. The unit of analysis used was the sentence level. The manifest (the obvious meaning of the words) and latent content (the underlying meaning of the interaction that may not be specifically stated but can be derived from the context) were evaluated.
When the interviews were completed, the transcripts were first examined to identify commonalities and then to code the relevant information and categorize it. Categories were comprised of data that were similar. Three categories established were (1) the type of service for the individuals (career, volunteer, or hybrid); (2) the type of mental health services available; and (3) the presence of the “Superhero Effect” (to be discussed later). Random names were assigned to the transcripts of the interview so they could be referenced in the report while protecting their identity.
Themes
A few themes played a key role in the final determination of the effects of the mental health stigma. Four main themes came up in all of the interviews: the type of service, the type of mental health services available, the Superhero Effect, and the use of alcohol to escape from the pain.
Results and Discussion
Descriptive Statistics. Table 1 describes the eight participants. Age, race, and ethnicity were not recorded.
Discussion of Themes
1. Type of Fire Service
The type of service (career or volunteer) in which the individual served was one of the most common factors mentioned. The three career individuals felt comfortable that their department was moving in the right direction with providing mental health services to its employees. However, all three did not feel that their departments were combating the cultural stigma against mental health treatment. Larry, for example, had to stand up in a room among 100 fellow firefighters and tell his department chief that its mental health program was a failure because he was living proof.
Larry said that he was able to talk with his shift about his problems only after he froze at an incident scene. He experienced a mixture of cultural and self-stigmas prior to his breaking point. Once his shift understood what he was going through, the cultural stigma no longer existed in his shift, leaving his self-stigma.
Jared described the fire service as a Type A personality environment where any deviation from the norm is considered weakness. He believed that atmosphere was responsible for the cultural stigma.
In the volunteer service, there is no consistency in working with fellow firefighters. In a career department, you know the people with whom you are working; volunteers know who their partners for the call will be only when the alert is sounded.
Josh described the volunteer side of the fire service as an “If you can’t handle it, get out” environment. There is less support from peers because an individual does not spend every shift with the same people. Josh, the one hybrid department firefighter in this study, expressed that a cultural stigma against mental health exists in his career and volunteer departments and that anyone who does less than what is expected is labeled as weak.
Colleen, a volunteer, noted that the expectation in her department is that you do not bring your problems to the fire department because it will affect how others view you. There is the cultural stigma against mental health, and people do not feel free to talk about what they are going through.
John, a volunteer firefighter, revealed that his department has the stigma and that mental health has never been spoken about seriously in his department in the three years he has been a member; it is mentioned only in a derogatory sense—making fun of mental health.
2. Type of Mental Health Services
All participants said there is a lack of assistance in their departments. Career departments are doing a better job of providing some resources to their employees; volunteer departments provide little to none.
In career departments, services are more easily accessed. However, in Larry’s case, the services seemed good at the initial meeting; but now a year later, he realizes how poor the service his department made available was. Larry was seen by a peer support group he described as unorganized and amateur. After the first meeting with the peer support group, Larry never had a follow-up; nor was he passed on to a more experienced provider. It was simply one meeting and nothing else. When he informed his county fire chief that the services available were failing the department, his chief asked him to be a part of a committee that would search for better services to offer the department. However, he still believes that if his situation repeated itself, nothing would be changed. He has little faith in his department’s services. He acknowledged that his department has the right intention but that the higher-ups lack the knowledge to address this problem.
Josh (hybrid department) explained that the only service of which he is aware in his career department, after working there for more than five years, is a critical incident stress management (CISM) team. There has been no mention of any other available services. He related that his shift deals with the horrors of the job by just talking to each other. He and his normal partner on the ambulance sit in the back of the unit and talk about whatever is going on in life—that is their mental health assistance.
Josh added that he has no clue as to what, if any, mental health services the department provides for volunteer members. This story, unfortunately, was the same among the volunteers interviewed. John, whose volunteer department is near a large city in the greater Washington, D.C., area and responds to numerous fatalities every month, has no mental health services for its members. John noted the extent of the assistance: “There is some ‘debriefing’: ‘Is everyone okay?’ It’s never much more than that.” The entire county is volunteer, John says, and he knows for a fact that none of the other departments in the county offer any mental health services.
James, who has been a volunteer for 14 years, describes his county’s mental health program as a broker service. His county provides for the volunteers the same employee assistance program (EAP) it offers to its career firefighters. His experience with the program, he reported, drove him to the point of not even seeing a counselor. He had let the horrific sights build up for 13 years before he asked for help. When he did ask for help and called the EAP, he requested an experienced trauma/PTSD professional who was familiar with the fire service. The EAP told him it did not offer experienced professionals, only people who have dealt with PTSD once or twice. James abandoned his attempt to seek assistance.
James said that when he became involved in a CISM debriefing by a team comprised of other volunteers in the county, the process did not solve anything for him; it made things worse, and there was no follow-up.
Sadly, neither the career nor volunteer members interviewed came from departments that were proactive in this matter. According to this survey, the career side came off slightly better in regard to services available, and the volunteer side is clearly lacking in services, which is in great part caused by a lack of funding. Volunteer department participants who came from a county-run structure that included career personnel could access the EAP in the county. Volunteer departments that relied on their own funding did not offer any type of assistance.
All the participants shared a view that would greatly help in this fight against the stigma and for better assistance programs. Usually EAP providers have worked with PTSD or trauma before, but the eight participants prefer counselors who know the fire service, are available so people can get to know them, are familiar with the stigma firefighters face, and have extensive experience treating PTSD. John mentioned that a professional who does not know the fire service does not fully understand what firefighters go through daily, which may present barriers when working with firefighters.
3. The Superhero Effect
This project revealed that members of the fire service think of themselves as “superheroes”—that they are incapable of being hurt. Part of the reason for this could be that advances in technology have made it possible for firefighters to do so much more today than ever before. This Superhero Effect of being physically invincible, however, has led to the idea that firefighters are exempt from being hurt mentally as well.
Firefighters and EMTs have equipment to protect them from the outside environment that threatens their lives, but this equipment can fail at a given temperature or simply by being cut by a sharp object. The equipment protects firefighters’ bodies for a given amount of time. However, no amount of protective equipment can protect a firefighter’s mind from the horrific images seen in this profession.
The Superhero Effect was noted by all the participants. Larry, for example, stated: “The number one thing we need to do in the fire service is to stop thinking that we are Ironmen.” This mentality of invincibility stems in part from the cultural stigma against mental health. As David (volunteer) noted: “To be in the fire service, you have to be tough to be able to handle the horrific sights you see because nobody wants to be labeled as weak. Often, firefighters push [it] under the rug and move on.”
4. Covering the Pain
Some participants said they used alcohol to escape the pain of the memories. Larry began using alcohol years before he asked for help. The night of the call that sent him over the edge, he threatened to stop at the liquor store and buy a fifth of scotch if his captain sent him home. Even after he had seen the peer support group, he said he drank so much to drown out the memories that he lost his family and almost committed suicide. He endured all of this to drown out the memories because he was afraid of being labeled weak and because the services originally provided to him were inadequate.
Josh reported: “As soon as I get home from my shift, I drink like a fish … anything that will alter your mind because you start thinking about that kid you just were doing CPR on, collapsing his chest to his back ….”
This finding of turning to alcohol to cover up the memories is not new to the fire service. In their article, P.J. Norwood and James Rascati state: “Alcohol abuse has been and continues to be an issue for both career and volunteer firefighters. It is estimated that the alcohol abuse disorder rate is seven to nine percent for adult Americans and anywhere from 25 to 30 percent for firefighters. Alcohol abuse has been a culturally accepted way to deal with the stress inherent in our profession. Prior to the advent of EAP, critical incident debriefing, or other counseling services, some firefighters dealt with stress by self-medicating with alcohol.”20
The shocking fact is that turning to alcohol has become “culturally accepted.” (20) The fire service has a culture of not changing things unless it is broken, as described by several of the study participants. John described the fire service as an “If it’s not broken, don’t fix it” type of culture. This could be a contributing factor to the stigma against mental health; some may think that mental health is something new that is replacing something that is not broken.
The NFFF notes that suicide ideation and attempt are “almost three times as likely in the presence of alcohol abuse or dependence.” (8) The covering up of the memories by using alcohol has increased the potential for firefighter suicide. Covering up the pain makes the problem worse and increases the chance of the individuals’ losing more than just their happiness.
Study Conclusions
This study shows that the stigma against mental health in the fire service is a combination of a self and a cultural stigma. Each participant expressed times when there was a strong cultural stigma against mental health in their department. They also said there were times where they created the stigma themselves because they were scared of being labeled.
The self stigma is created by an individual because the person is afraid that someone will label or judge him if he asks for help. This creates fear in an individual even if the individual does not know whether the cultural stigma exists in the environment. The person is too scared to ask for help. When this happens, an individual cannot even begin to know what services are available to help. This type of stigma may lead an individual to cope with the issue through other methods, possibly alcohol or other means.
The cultural stigma derives from an individual’s shift, station, or department. Every member of the shift, station, or department does not have to share in the continuation of the stigma: It is upheld by those who voice their opinions the loudest. Unlike the self stigma, where individuals do not know for sure if they will be judged or labeled, the individuals know for sure that the cultural stigma will result in the individuals’ being labeled and judged because these individuals have seen the dislike for mental health displayed on a regular basis. This type of stigma may cause individuals to turn to other methods of coping with the memories because they will likely be less willing to ask for help.
Not all study participants responded to the question, “What does the fire service need to do to be more accepting of mental health?” The responses noted basically said, “Create awareness and introduce mental health early on.”
All of the participants reported that there was little to no discussion about mental health or the sights they might see in the basic firefighter or EMT classes. Edward, a new volunteer, stated mental health in the fire service was covered “maybe an hour tops out of a 167-hour firefighter 1 class.” All participants cited the lack of adequate discussion.
The creation of awareness programs in the fire service would create a friendlier environment for mental health. Programs would encompass discussions about mental health. Once members are made aware of the detrimental effects of the stigma on individuals, only then can departments begin to destigmatize the culture in its ranks.
This research project was limited to eight individuals. Therefore, it cannot begin to determine what every individual struggling with this stigma is experiencing. Further research is needed to determine what mental health services are best suited for the fire service and to explore ways departments can address this crisis. Additionally, further research is needed on the Superhero Effect, to determine if this is a fire servicewide mentality or just relevant to the eight participants and on identifying other means by which firefighters are trying to cover up their memories besides alcohol and joking. I have begun planning research projects on the final two items.
References
1. National Fire Protection Association. n.d. “NFPA Reports–The Fire Service.” Retrieved Oct 19, 2016a (http://www.nfpa.org/news-and-research/fire-statistics-and-reports/fire-statistics/the-fire-service).
2. National Fire Protection Association. n.d. “NFPA Statistics–Fire Department Calls.” Retrieved Oct 19, 2016b (http://www.nfpa.org/news-and-research/fire-statistics-and-reports/fire-statistics/the-fire-service/fire-department-calls/fire-department-calls).
3. Chen, Yong-Shing, et al. 2007. “The Relationship between Quality of Life and Posttraumatic Stress Disorder or Major Depression for Firefighters in Kaohsiung, Taiwan.” Quality of Life Research : An International Journal of Quality of Life Aspects of Treatment, Care and Rehabilitation 16(8):1289-97.
4. Hom, Melanie A, Ian H Stanley, Fallon B Ringer, and Thomas E Joiner. 2016. “Mental Health Service Use among Firefighters with Suicidal Thoughts and Behaviors.” Psychiatric Services 6(67):688-91.
5. Stanley, Ian H, Melanie A Hom, Christopher R Hagan, and Thomas E Joiner. 2015. “Career Prevalence and Correlates of Suicidal Thoughts and Behaviors among Firefighters.” Journal of Affective Disorders; 187:163–71.
6. Stancil, Lamaur. 2016. “Veteran IRC Firefighter Commits Suicide Shortly after PTSD Post on Facebook | Photos.” Retrieved (http://www.tcpalm.com/story/news/local/indian-river-county/2016/10/16/indian-river-firefighter/92198338/).
7. NBC Miami, n.d. “Treasure Coast Firefighter Commits Suicide Days after Discussing PTSD in First Responders, NBC 6 South Florida.” Retrieved October 20, 2016 (http://www.nbcmiami.com/news/local/Treasure-Coast-Firefighter-Commits-Suicide-Days-After-Discussing-PTSD-in-First-Responders-397453891.html).
8. National Fallen Firefighters Foundation. 2011. “Issues of Depression and Suicide in the Fire Service.”
9. Firefighter Behavioral Health Alliance. n.d. “What Are These Numbers? “Firefighter Behavioral Health Alliance.” Retrieved November 23, 2016 (http://www.ffbha.org/what-are-these-numbers/).
10. Henderson, Sarah, Vincent Van Hasselt, Todd LeDuc, and Judy Couwels. 2015. “Firefighter Suicide: Understanding Cultural Challenges for Mental Health Professionals.” Nova Southeastern University.
11. Britt, Thomas W, Tiffany M Greene-Shortridge, and Carl A. Castro. 2007. “The Stigma of Mental Health Problems in the Military.” Military Medicine; 172(2):157-61.7. 10.
12. Kim, Paul Y, Thomas W Britt, Robert P Klocko, Lyndon a Riviere, and Amy B Adler. 2011. “Stigma, Negative Attitudes about Treatment, and Utilization of Mental Health Care among Soldiers.” Military Psychology 23(1):65–81.
1 3. Kim, Paul Y, Jeffrey L Thomas, Joshua E Wilk, Carl A Castro, and Charles W Hoge. 2010. “Stigma, Barriers to Care, and Use of Mental Health Services among Active Duty and National Guard Soldiers after Combat.” Psychiatric Services 61(6):582–88.
14. Moffitt, Jenna, Janet Bostack, and Ashley Cave. 2014. “Promoting Well-Being and Reducing Stigma About Mental Health in the Fire Service.” Journal of Public Mental Health 13(2):103–13.
15. National Volunteer Fire Council. 2012. Suicide in the Fire and Emergency Services.
16. Heitman, Steven. 2016. “Suicide in the Fire Service: Saving the Lives of Firefighters.” Naval Postgraduate School.
17. Scimecca, JA. 1977. “Labeling Theory and Personal Construct theory: Toward the Measurement of Individual Variation.” J of Criminal Law and Criminology; 68(4):652.
18. Haynes, Hylton J. G. and Gary P. Stein. 2016. U.S. Fire Department Profile – 2014. Heitman, Steven. 2016. “Suicide in The Fire Service: Saving The Lives of Firefighters.” Naval Postgraduate School.
19. Dixon, Jeffery C., Royce A. Singleton, and Bruce C. Straits. 2016. The Process of Social Research. New York, New York: Oxford University Press.
20. Norwood, PJ and James Rascati. “Recognizing and Combating Firefighter Stress Recognizing and Combating Firefighter Stress.” Fire Engineering, December 2012.
Christopher L. McKenna has been in the fire service for seven years as a volunteer firefighter/EMT with the Vigilant Hose Company in Emmitsburg, Maryland. He has bachelor degrees in criminal justice and sociology from Mount St. Mary’s University. He is pursuing a master’s degree in forensic studies with a concentration in computer forensics from Stevenson University.

