From First Aid to Paramedic Service —Growth Pains in A Dallas Suburb


“Carrollton One to 287.”
“287 to Carrollton One—go ahead.”
“This is Carrollton One. We need a doctor of medicine stat.”
“Carrollton One, this is Dr. Jones, go ahead.”
“ Doctor, we have a CPR in progress. The patient is a known heart patient taking nitroglycerine and inderal. We have the patient intubated and have started an IV of D5W TKO. Right now, the patient is in ventricular fibrillation. Request permission to defibrillate at 300 watt seconds.”
“Carrollton One, send me a strip. I read ventricular fibrillation also. Go ahead and defibrillate at 300 watt seconds. Defib at 300 watt seconds again. Continue CPR and give the patient two amps of sodium bicarbonate followed by .5 mg epinephrine IV push.”
“ Doctor, sodium bicarbonate and epinephrine are on board.”
“Hold CPR 5 seconds and send me a strip. Defibrillate at 400 watt seconds. Defib at 400 watt seconds again. Give 100 mg. Lidocaine 1 percent IV push.”
Change in condition
“Doctor, his rhythm has converted to ventricular tachycardia and he remains unconscious. We have stopped CPR and are attempting to take a blood pressure. Doctor, we have a BP of 80 over 68, but he still is in a ventricular tachycardia at a rate of 140 a minute.”
“That’s what I read Carrollton One. Defibrillate at 50 watt seconds.”
“Doctor, the defibrillation has converted the patient to a sinus rhythm at a rate of 80 a minute.”
“Carrollton One, start a 4 percent lidocaine drip and flow it at 3 mg. a minute. What is the patient’s neurological status?”
“Doctor, the patient is still unconscious. Blood pressure has risen to 118 over 84. Respirations are 16 a minute.”
“Ok, Carrollton One. Give the patient 3 liters per minute oxygen.”
“Carrollton One—what is your destination and estimated time of arrival?”
“We’ll be en route to Plano General. ETA will be 15 minutes.”
Thus, another life was saved by the advanced life support skills of Carrollton Fire Department paramedics.
Roots of paramedic service
Prior to the inception of the paramedic program in 1976, all ambulance calls were handled by emergency medical technicians. These EMT’s could provide only basic life support consisting of bandaging and splinting, airway maintenance, supplemental oxygen administration and cardiopulmonary resuscitation.
They were the second phase of an evolutionary process that started in 1970 when the CFD took over the ambulance service from the local funeral home. At the time of this takeover, CFD personnel who were to ride the ambulance were given eight hours of medical training. These first-aid attendants had no training in CPR. Then in 1976, with the adaption of the paramedic program, emergency medical services were expanded to include advanced life support techniques and procedures. City fathers of Carrollton, a suburb of Dallas, allocated funds for the paramedic program, because of the success and popularity of the Dallas Fire Department program established in 1972. Training for paramedics in the Dallas County area was provided at the University of Texas Health Science Center, adjacent to Parkland Memorial Hospital in Dallas.
Three-month course
The program, directed by Dr. Thai and Dr. James Atkins, a nationallyrecognized cardiologist, was a thorough three-month course open to state-certified EMTs. Advanced life support techniques were taught here that had rarely been seen outside a hospital emergency room. These practices included intubation, electrocardiogram analysis, intravenous drug therapy, electrical defibrillation, blood volume replacement and mechanical aids.
Intubation is the practice of inserting a long plastic tube in a patient’s airway to prevent the patient from choking on his stomach contents. This is a common danger in an unconscious victim and more especially a heart attack patient.
The heart attack patient must also be monitored by an electrocardiogram. From this ECG, the paramedic will determine the patient’s heart rhythm and the appropriate drug therapy. Most drugs carried on a paramedic ambulance are used to convert an irregular heart rhythm. Sometimes electrical defibrillation must be used with drugs to get the heart beating after it has stopped.
Unlike heart attack patients, the victim of shock needs volume replacement of his depleted blood. Fluids may be given intravenously, as most paramedic drugs are given, or volume replacement may be accomplished mechanically by the use of military antishock trousers. When inflated with air, these rubber trousers divert blood flow from the legs to the vital organs.
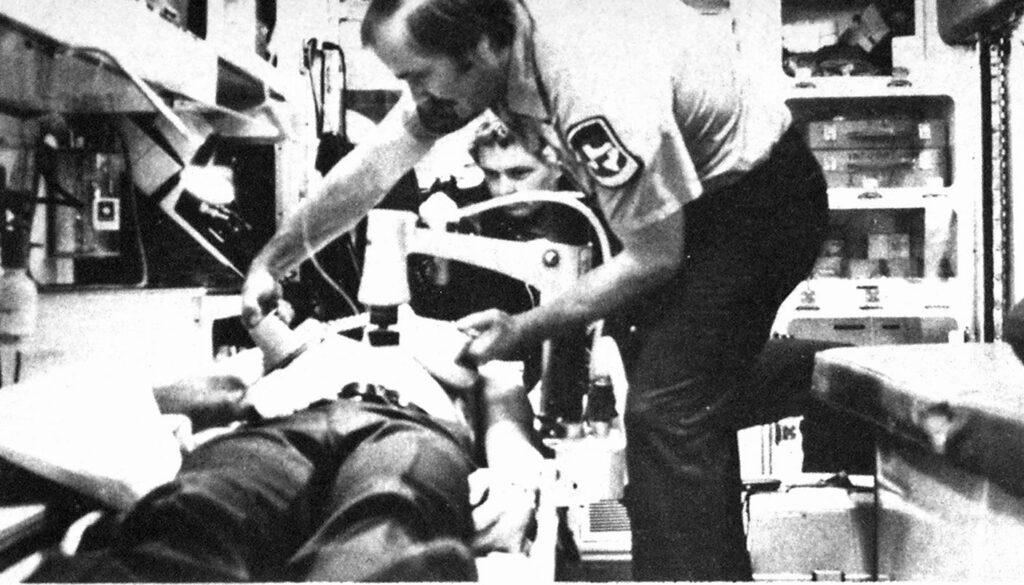
Both the shock patient and heart attack patient may suffer heart failure; thereby requiring CPR. The greatest mechanical aid available to the paramedic is the mechanical thumper, which performs mechanical CPR without interruption. It makes IVs easier to start by opening collapsed veins, and is much more efficient than manual CPR.
Problems expand
This expansion of emergency medical services also expanded the problems associated with the EMS system. For example, at the start of the paramedic program, the public did not understand what was being done to the heart attack patient in the back of the ambulance. Accustomed to the old days of “lift and tote,” they did not realize that the paramedic was stabilizing the patient’s condition before transporting him. As the public’s exposure to paramedics has increased over the years, this has become less of a problem.
However, other segments of the populace view the advanced life support ambulance as a taxi service for colds and other nonemergency calls. If the ambulance were to handle this type of call, it would not be available for major emergencies, such as heart attacks. Therefore, nonemergency patients are encouraged to seek private conveyance to the hospital. This situation also is being remedied by the public’s exposure to Carrollton’s paramedics.
Because Carrollton was the first suburb in Dallas County to develop its own paramedic program, its paramedics were faced with many unique problems. Primarily, these difficulties may be divided into the following categoriesforganizational, working relationships, supplies, and equipmental considerations.
Second paramedic added
Organizationally, the situation was a three-fold dilemma. At first the ambulance was manned by only one paramedic. During a CPR, it was difficult for one paramedic to talk with the doctor by radio, intubate, start an IV, push drugs, defibrillate and monitor an electrocardiogram by himself. The obvious solution was to man the ambulance with two paramedics. This delayed solution was implemented when vacancies were finally available in the Dallas paramedic training school.
The second organizational dilemma was the paramedic’s position in the fire department. When fire department positions were established by state civil service law, the paramedic position did not exist. Because of the knowledge and skills required, the City Civil Service Commission authorized a $100 educational allowance per month for all paramedics. This bonus placed a paramedic’s salary above a driver position and below that of lieutenant. Theoretically, a man could be promoted from paramedic to lieutenant without holding the driver’s position, because of a state civil service law stating that elegibility for promotional advancement is based on pay grades rather than rank. Although this situation never arose, the possibility alienated many drivers.
Another positional problem arose when a second driver rank was created two years after the start of the paramedic program. The original paramedics had been promised that after two years of riding an ambulance, they would be free to take the driver’s examination. Therefore, the intial paramedics were given second driver status, in accordance with the agreement, without having to take a competitive exam. Thereafter, they took written competitive promotional exams along with non-paramedic personnel.
Protocol involved
However, interpersonal difficulties are not limited to the fire department. Because the doctor is not at the scene, the paramedic becomes the eyes and ears of the doctor, and sometimes he must be more than that. Paramedics have a protocol of standing orders for the administration of all drugs that they carry. However, as an agent of the doctor, they must have his permission to start an IV, administer drugs, intubate or defibrillate.
If a paramedic were to follow a doctor’s orders that was inconsistent with his protocol, he would be as guilty as the doctor of malpractice. Therefore, if a doctor inadvertently gives a wrong order, the paramedic must ask the doctor to repeat the order. As a last recourse, the paramedic may ask for another doctor.
When a physician does not listen to a paramedic’s collected patient history, the paramedic must diplomatically question the doctor as to what knowledge the doctor wants. Finally, some doctors are not familiar with certain paramedic equipment, i.e., military anti-shock trousers and the mechanical CPR thumper. Because of this unfamiliarity, they do not use this equipment. Again, the paramedic must educate the doctor in its use.
Obtaining supplies
The supplying of equipment can also be a problem. At the inception of the paramedic program, most drugs were supplied in glass ampules. Syringes, needles, and ampules were all packed individually. The syringe would have to be combined with the needle to draw out the drug after the ampule was broken. This was time-consuming for one paramedic to do with each individual drug during a CPR. Nowadays, most cardiovascular drugs are supplied in a cartridge-type syringe that is much quicker to set up.
The time element was also a problem in that certain drugs were ordered from out of state. This situation was corrected by contacting the Dallas Fire Department supplier and borrowing from the D.F.D. until an in-state supplier could be found. The final supply consideration was the concept of revenue sharing. A municipal association of governments in the North Texas area provided funds for the purchase of a radio for hospital communications. Because the radio did not arrive until months after the promised date, the department was forced to buy a radio from its own funds.
Another area of concern was equipment malfunctions. Carrollton radio signals were not easily picked up at Parkland Hospital due to the distance. Also, certain radio dead spots existed within the city where no signal whatsoever could be received from Parkland Hospital. In this situation, the ambulance would have to be moved 100 yards in one direction or another.
Second alternator installed
Perhaps, the most common mechanical failure was the inability of the ambulance to provide adequate electricity for its appliances. After many experiments, a second alternator and a second battery were added to the ambulance. This cured the electrical problem.
Despite all the problems involved, the paramedic program has generated substantial positive publicity for the fire department. Concerned citizen groups have donated equipment for the paramedic ambulance, such as MAST trousers. Carrollton paramedics teach CPR to the general public at the fire stations. More and more area businesses are asking for first aid on-the-job training for their employees. Paramedics have helped the CFD training officer certify fire fighters as EGAs and EMTs. The police department uses fire department paramedics extensively to check out prisoner injuries.
However, the most important aspect of the paramedic program is the advanced life support that is now given at the scene rather than at the hospital. There is no way to estimate how many minor heart attacks have been prevented from becoming major ones. Many heart patients are alive today because a paramedic ambulance was there when they needed it!


