Medical Responsibility in Disaster Manaaement
FEATURES
DISASTER MANAGEMENT

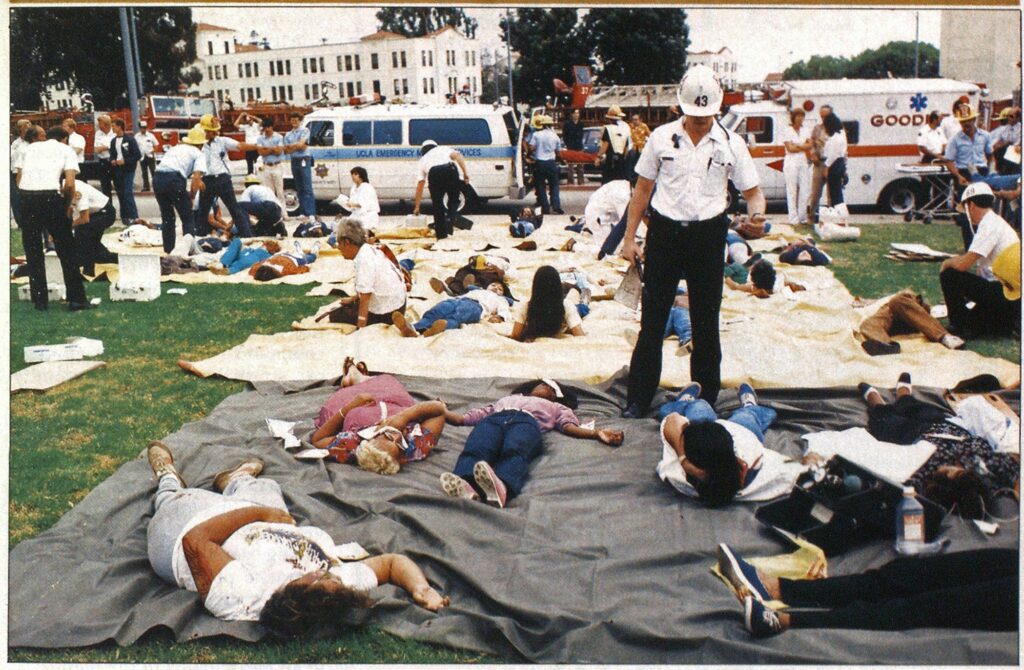
Photo courtesy of Los Angeles City Fire Department
The management of mass casualties at disaster scenes is an often addressed topic at emergency medical services (EMS) meetings throughout the country. EMS includes not only the medical community, but all of the allied emergency professions and agenciesr A catastrophe can happen anytime, anywhere. The large metropolis, the small city, the remote rural area are all potential settings. Emergency personnel must be ready to deal with any situation, large or small, natural or man-made.
This article on medical responsibility in a disaster is based on both my own personal experience and an aggregate of opinions of medical authorities in the United States.
A disaster is defined as an incident that taxes or puts additional demand on an existing emergency system. It does not have to be of the magnitude of the MGM Grand Hotel fire (Las Vegas, NV), the Hyatt Regency Hotel collapse (Kansas City, MO), or the Clinton, MO, gas explosion and fire that leveled an office building and a section of the city square.
An efficient disaster plan is integrated with fire, police, medical, and allied agencies, and civilians from the public and private sectors. The plan must be realistic, relatively basic (not specifically sophisticated), and workable.
A relatively recent innovation has been to include the fire service in medical disaster planning. It has taken the medical service several years to accept this “mutual aid,” something that the fire service has known and practiced for years. We must rely and depend on mutual aid response and a pooling of community resources into one efficient medical assistance system.
Physicians, basically, are accustomed to attending to people on a one-to-one basis, not to groups of people at one time. When disaster strikes, the physician is put in a totally different situation than that which he is accustomed to. Multiple casualties and multiple medical challenges require rapid, on-scene, cursory, rather than definitive judgements and decisions. This reinforces the necessity of the allied emergency services.
All too often, it is assumed that a physician can provide order and direction in a disaster situation. This is a misconception. Nowhere in the discipline of medical training is there an introduction to disaster and casualty management. The role of the physician is not to direct care but to deliver care.
There is one unbreakable rule: One person must be in charge. Call him what you may, triage officer, chief executive officer, disaster officer, etc., but one person must be in command. Assuming command can stress the medical community because routinely a physician gives orders and advice; he is not used to taking them. However, in my experience, I have found that most physicians who are called into a disaster situation are glad to have victims directed to them! In organizing your mass casualty management plan, it must be determined prior to, not after, the disaster that one person will be in command, and this must be made clear to all participants in the plan.
The paramount principle of disaster management is that of advanced planning or pre-planning. This is where the medical community must work in concert with allied health and emergency personnel: fire, police, paramedics, EMTs, nurses, and basic life support teams, including civilian and military personnel. These people must help provide coverage at the disaster site. Their arrival and operations must be pre-planned, preordered, and thoroughly trained for. Their overall and specific objectives and responsibilities in the plan must be clearly defined.
The medical officer need only coordinate medical activities. These he coordinates at the scene with the chief operational commander and works in conjunction with fire, police, and other agencies to assure efficient emergency medical care. Depending upon the scope of the disaster, he may or may not be responsible for triage.
The triage officer at the scene need not be a physician. But neither should the receiving hospital be the primary triage area. Basic triage should be done prior to transporting victims to the health care facility. The definitive triage may be performed at the hospital receiving area. The medical community should be well-versed in the following four categories of triage:
- Category 1—essentially no EMS personnel are needed. This covers civilians at the incident scene who sustained only minor injuries and can seek medical attention for themselves and for one another (known as the “buddy system”).
- Category 2—minor medical attention is needed. Basic wound care, dressings, tetanus immunizations, etc., are given. This can easily be handled by paramedics.
- Category 3—seriously injured persons needing major medical attention. This requires the presence of medical and paramedical personnel and all other resources or involved agencies that are available. The hospital’s role comes into play here. The hospital disaster plans must be implemented. Their arrangements with specialty institutions for specific injuries (burns, head injuries, toxicity cases, etc.) and transfer agreements, if necessary, must be utilized.
- Category 4—victims who will die. Though no one wants to accept this, there are those who will not survive. Again, we must be realistic, no matter how it hurts. These victims will need comfort for their impending demise. This service too must be pre-planned.
Remember that no triage officer is perfect. He too will make mistakes, and may have to decide on patient placements, upgrading them or downgrading them, possibly after many re-assessments.
The aftermath of disaster operations are too often overlooked. Once the disaster is contained and victims are hospitalized, too often “finish” is written to the episode. This is an error. The physical and psychological impact on all of us in the emergency services can leave lasting impressions that are difficult to cope with. Dollars do not remove the scars and imprints.
Psychological support is a necessity and should be the rule, not the exception. Personal and group counseling is often necessary. We need to talk, to help understand, to vent hostilities, anxieties, praise, love, affection, and concern. We need a sounding board, an ear to listen, a person to talk with, not to. I’m not talking about “bull” sessions, but professional counseling sessions as well as dialogue with co-workers. Postmortems (general and specific critiques) are necessary ingredients in the total spectrum of crisis management. In emergency services, mental and psychological health is just as important as physical well-being.
This short treatise has only been to project the medical responsibility in a disaster. The total scope of organizational responsibilities in a crisis is great, with all areas of emergency services participating. The integrated system of all agencies and the team approach is of paramount importance. Basically, it comes down to: PLAN THE WORK, WORK THE PLAN.

