By Terry L. Von Thaden
Although recent studies have focused on quantifying and evaluating sleep in the workplace, scientific modeling and prescriptive solutions have done little to help change the culture of embedded social habits interfering with sleep that pervade the firehouse and may diminish firefighter health. Controlling fatigue has long been an issue in the fire service, in part because of 24-hour shift scheduling and calls for assistance around the clock. Some firehouses have recently added Fatigue Risk Management programs to promote awareness and fatigue-mitigation strategies, but many agencies still do not take advantage of evidence-based practices for reducing fatigue and increasing alertness in the workplace. This article discusses some of the latest research on the long-term physiological effects of fatigue to raise awareness in the fire service and provides information toward gaining a tactical advantage over fatigue on duty days and days off.1
Effects of Fatigue
Fatigue can lead to poor decision making, reduced skills performance, poor hand-eye coordination, and increased reaction time, all of which can increase risk and the potential for an injury or accident. But beyond that, sleep habits in modern society may be harmful to your health. For instance, the leading causes of death in the fire service, cardiovascular events and vehicle accidents, both can have origins in fatigue.
Fatigue has many definitions. For the purposes here, fatigue is described as a reduced mental and physical state resulting from insufficient or poor quality restorative sleep. Not only does compromised sleep increase propensity for error, but it also contributes to deleterious physiological changes in the body.

Humans have evolved on a planet with systematic light and dark cycles occurring on a 24-hour, or circadian, basis. The human body biologically reacts to these circadian cycles with changes in behavior and physical and cognitive abilities. Circadian rhythm dips and rises at certain points throughout the day to regulate wakefulness and sleepiness. Humans synchronize their internal circadian clock each day with cues from the light and dark cycles. The physiological responses in the body – such as core temperature, hormone levels (e.g., melatonin and cortisol), eye movement, and alertness, to name a few – have adapted in response to these cycles over time.
Circadian dips and rises, known as the circasemidian rhythm, have a two-peak daily pattern caused by the circadian rhythm as it processes through two cycles per day. Circasemidian rhythm has been measured in many studies of performance and physiological activity. Although individuals vary on whether they are a morning-personality type (early birds, larks) or an evening-personality type (night owls, ravers), the circasemidian rhythm generally rises and creates a drive for alertness between 0900-1100 hours (morning wakefulness) and 2100-2300 hours (the second wind); it dips between 0200-0600 hours (the window of circadian low) and 1300-1500 hours (the post-lunch dip) each day, creating a strong drive for sleep. These dips are expressed more intensely if a person is sleep deprived (Table 1).
The Sleep Process
The sleep process comprises a series of 90- to 120-minute cycles that repeat throughout the sleep period. Each cycle consists of two phases – Rapid Eye Movement (REM) and Non-Rapid Eye Movement (NREM) – conducted in four stages. During REM sleep, which constitutes ~25 percent of a normal sleep cycle, the body experiences almost complete immobility as muscle control is relaxed in a response known as atonia. REM sleep is a time when information is stored into memory and people may experience intensive, vivid dreams. People in REM sleep are usually easy to awaken. In NREM sleep, which constitutes ~75 percent of a normal sleep cycle, the brain slows, body temperature drops, blood supply to the muscles is increased, tissue growth and repair happen, and hormones are released. People in NREM sleep are disengaged from the environment and are often difficult to awaken. If awakened in NREM, people complain of grogginess.
During wakefulness, brain activity is comprised of low-amplitude, high-frequency brain waves. A person entering Stage 1 sleep enters the phase between consciousness and sleep, often referred to as twilight sleep. Brain activity is comprised of low-amplitude, mixed-frequency waves. Stage 2 sleep is marked by higher-amplitude waves, K-complex waves (a high-amplitude negative wave followed by spikes), and sleep spindles (short bursts of high-frequency oscillations). K-complex waves and sleep spindles are unique to the first sleep stages and work to suppress stimulus response and aid in memory consolidation.
Muscle twitches, followed by a sleep spindle, often occur in these lighter stages of sleep. It is largely hypothesized that this relationship between muscle twitches and sleep spindles represents the nervous system reinforcing and organizing neural pathways, the brain/spinal cord/muscle connection.
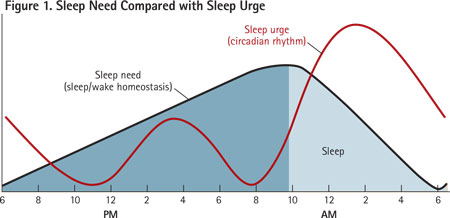 |
| The black line depicts sleep need, which rises through the waking hours and decreases during sleep. The red line depicts a normal circadian rhythm wherein sleep urge is greatest at night; there is also a slighter increase at midday (post-lunch dip). |
A person entering Stage 3 sleep moves into deeper sleep with slower brain waves. Stage 4, thought to be the most restorative stage of sleep, is characterized by high-amplitude, low-frequency brain waves; decreased body temperature and blood pressure; and sympathetic nervous system activity, along with decreased cerebral glucose use. It is in these deeper stages of slow wave sleep (SWS) where the body makes repairs. SWS contributes to the inhibition of the stress hormone cortisol and assists in the release of growth hormones, allowing cell growth and regeneration.
Once past Stage 4 sleep, the body proceeds back through the sleep stages into lighter sleep and REM, and then the entire cycle begins again. As the sleep cycles continue through the sleep period, less time is spent in deeper-stage sleep and more time is spent in lighter-stage sleep. Stage 2 sleep is typically where most time is spent in a sleep period overall.
The biological circadian processes of the body signal it to sleep. Normally, a person needs about six to eight hours of sleep each day. This is slightly variable because of the length of the sleep cycle in individuals. Those who process through a sleep cycle faster require fewer hours of sleep to feel restored.
Ordinarily, melatonin, a hormone that reduces alertness, is released into the body a couple of hours prior to the usual bedtime. Melatonin is usually released toward nighttime, as humans are by nature a daytime species.
Sleep/Wake Homeostasis
The sleep cycle is regulated not only by our biological circadian clock but also by a sleep/wake homeostasis. Sleep/wake homeostasis is a drive that creates a balance between wakefulness and sleep. When a person has been awake for a number of hours (known as history of wakefulness), this homeostasis indicates that a need for sleep is building; the longer one remains awake, the more intense the need for sleep. This drive helps the body maintain enough restorative sleep to compensate for the hours spent awake.
As an example, Figure 1 depicts the 24-hour cycle of a person who wakes at roughly 0600 hours. As the person proceeds throughout the day, the need for sleep gradually increases until approximately 2200 hours, when the person experiences the greatest sleep need and subsequently retires to bed. At this point, the need for sleep decreases markedly with each hour until it has been mollified after approximately eight hours. Accordingly, the body’s natural circadian rhythm experiences several highs and lows throughout the 24-hour period regardless of sleep history.
Circadian Disruption and Health
Research has shown that people with disturbed body clocks and disrupted sleep cycles can suffer a myriad of health problems. Firefighters can suffer from acute (transient), cumulative, and circadian fatigue.
Acute. In an acute fatigue state, which normally occurs after a wakeful period of longer than 16 hours, a person experiences diminished mental capability caused by prolonged, continuous wakefulness between two major sleep periods. This is seen as a transient performance decrement and is usually eliminated after one good-quality, nocturnal sleep period.
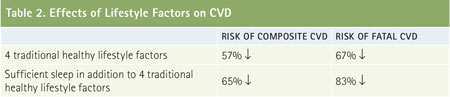 |
| This chart shows the relative risk of CVD in a longitudinal study of 17,887 people, which compared those with traditional healthy lifestyle factors to those with one or none. The addition of sufficient sleep alone remarkably decreases the risk of a cardiovascular event. |
Cumulative. In a cumulative fatigue state, a person experiences diminished mental capability caused by disturbed or shortened major sleep periods between two or more successive major waking, duty, or work periods. One major sleep period will not eliminate cumulative fatigue.
Circadian. In a circadian fatigued state, alertness and performance are reduced during night hours, particularly during the window of circadian low. Although there are numerous reasons for circadian disruption in the firehouse, common reasons are shiftwork scheduling, irregular sleeping patterns caused by workload (calls) or noise, wakefulness at night, and sleep issues such as sleep apnea and insomnia.
Metabolic Syndrome
Aside from cognitive issues, diabetic response, decreased metabolic function, and weight gain are concerns since sleep contributes to hormone release, glucose regulation in the body, and cardiovascular function. As little as two nights of disrupted sleep can increase insulin resistance in the body, a condition in which glucose builds in the bloodstream rather than being absorbed by the cells. Experienced over time, this insulin resistance can lead to Type II diabetes.
A primary contributor to insulin resistance is excess weight, particularly around the midsection. Excess midsection fat plays a part in chronic body inflammation, which can lead to additional serious health problems such as imbalanced cholesterol and cardiovascular disease (CVD). Hormones that control appetite and energy disbursement (i.e., leptin and ghrelin) have been linked to increased obesity risk and sleep loss. When individuals experience limited sleep, reduced leptin and increased ghrelin send signals to the body, reducing metabolic function and indicating hunger. Evidence indicates these effects are modifiable risk factors in our culture since increases in obesity and decrements in sleep duration over the past decades appear correlated.
Obstructive Sleep Apnea
Studies have also linked obesity to a higher risk of obstructive sleep apnea (OSA), a disorder where the airway becomes blocked and causes a person to stop breathing during sleep. A study by the Federal Motor Carrier Safety Administration found that the prevalence of sleep apnea increases with age and the degree of obesity. Untreated OSA can jar people out of a natural sleep rhythm up to hundreds of times a night. Accordingly, people spend more time in the lighter stages of sleep to the detriment of deep, restorative sleep. This may result in daytime sleepiness, cognitive decrement, and lost productivity. Increased attention to the diagnosis and treatment of OSA in the trucking industry has significantly reduced accidents over the past decade.
Gene Changes
In a recent study, blood samples were taken from individuals who after just one week of having fewer than six hours of sleep a night showed changes to more than 700 genes. In addition, some inflammatory, immune, and stress responses were detected in the subjects. This may at least in part help explain the serious health consequences linked to short sleep periods, such as obesity, heart disease, certain cancers, and diabetes.

Further, sleep deprivation destroys brain cells and prohibits the release of toxic proteins from the brain. Chief among them is amyloid beta, which is found in increased amounts in the brains of those with Alzheimer’s disease.
Cardiovascular Events
The authors of a 2012 article in The European Journal of Preventive Cardiology conducted a systematic review of available prospective studies investigating the association between insomnia and the risk of developing or dying from CVD. The studies involved 122,501 participants who were followed for three to 20 years. Insomnia, defined as difficulty of initiating or maintaining sleep or the presence of restless, disturbed nights, was assessed through a questionnaire. Throughout the 20-year follow-up period, 6,332 cardiovascular events occurred in the participants. A cumulative analysis of the studies showed that, all effects being equal, the participants who regularly experienced insomnia had a 45 percent increased risk of developing or dying from CVD during the follow-up period.
Equally, the MORGEN study (2013) found that sufficient sleep (≥7 hours) in conjunction with following the traditional lifestyle factors of sufficient physical activity, a healthy diet, (moderate) alcohol consumption, and nonsmoking, contributed to lower CVD risk. This study included a cohort of 8,128 men and 9,759 women, ages 20-65, free of CVD at baseline.
During 10-14 years of follow-up, 607 composite CVD events (fatal CVD, nonfatal myocardial infarction, and stroke) occurred, of which 129 were fatal. The participants who maintained the four traditional healthy lifestyle factors had a 57 percent lower risk of composite CVD and a 67 percent lower risk of fatal CVD compared with those who followed one or no healthy lifestyle factors. Sleeping sufficiently in addition to maintaining the four traditional lifestyle factors resulted in a 65 percent lower risk of composite CVD and an 83 percent lower risk of fatal CVD (Table 2).
Are Firefighters Setting Themselves Up for Failure?
Numerous factors contribute to disrupted and reduced sleep. Among them are culture, technology, light, diet and lifestyle, shift swapping, extreme changes in weather or temperature, stress, and sleep apnea. Following are some of the attitudes indicative of the more pervasive “alertness killers” in the fire service.
- “I’ll sleep when I’m dead.” Whereas on the one hand, some positive aspects of firefighter culture generate pride and provide a strong motivation to perform well, on the other hand, there are some negative aspects that instill in firefighters a sense of invulnerability. For many people, it’s a show of strength to go without sleep. Some feel they can get more accomplished if they reduce the time they spend sleeping. They see this as a harmless habit that illustrates endurance. For firefighters, the added cultural pressure to “suck it up” leads them to forgo sleep. Firefighters will often choose social life, other jobs, or training events over sleep on their off-shift days. We cannot change this culture overnight, but firefighters should do their best to curb these behaviors that induce a sleep deficit to protect their good health.
Unfortunately, the practice of trading shifts may result in firefighters being scheduled for more working hours than are “safe” and required for adequate cognitive and physiological functioning. Trading shifts allows for workplace flexibility, but many standard operating guidelines are vague about scheduling a maximum of back-to-back duty hours. Firefighters are expected to use their better judgment. The problem is that humans rarely recognize the signs of sleep deprivation: The more sleep deprived a person is, the less capable he is of seeing it in himself. The National Fire Protection Association guidelines discuss sleep loss and fatigue as related to other medical conditions; they do not recognize the fatigued state as a contributing medical condition. Developing and enforcing fatigue risk management policies in the firehouse, especially duty/rest guidelines, is a step toward changing the culture to recognize that reporting for work fatigued represents an occupational safety hazard.
- “You’ll pry my smartphone out of my cold dead hands.” Digital information and devices are ubiquitous: LED clocks, televisions, computers, smartphones, tablets, e-readers – all are part of modern life. The ability to binge watch a television series or quickly catch up on office business late into the night makes it too easy to disregard the fact that adequate sleep is necessary to function appropriately. Technology contributes to fatigue in that it has changed demands on our time. We now live in a 24/7 global society where information and technological interaction can be sought around the clock. Technology has been the largest contributor to fatigue over the past decade. Studies indicate that teenagers are sleeping up to five hours less per night than 10 years ago as a result of their interaction with technical devices. A technological determinism has been infused into today’s cultural expectations, such as the social obligation to quickly respond to text messages. This determinism has interfered with sleep just as much as the devices themselves.
Technological devices produce light, specifically blue light, which disrupts sleep. Research has shown that blue light increases alertness and suppresses melatonin, thus impairing the quality of sleep. In fact, this link is so strong that some are referring to LED light as a drug. Reading from an e-reader before bed not only makes it harder to fall asleep, but it also impacts sleepiness and alertness the following day. If you must use computers or other light-emitting devices in the evening, software or other technology that filters out the blue light may help. Digital clocks not only generate sleep-disrupting light output, but they may also increase anxiety, which is linked to habitually waking in the night and staring into the face of the clock. You can remedy this by turning the clock’s face away from view or blocking it out with a book or tissue box. Using the smartphone at night can also interfere with sleep; it can keep you mentally engaged late into the evening and make it hard to detach yourself from work so you can relax and ultimately fall asleep.
- “The fire service ruined my ability to sleep. I haven’t had a good night’s sleep in years.” Stress disrupts sleep. You can’t control the time an alarm comes or when hectic work pacing will occur throughout the day or night, but you can be aware that stress derived from irregular or random operational pressures may add to your sleep problems. Some stress is necessary to keep us stimulated, safe, and alert in the face of dangerous circumstances, but continual or chronic stressors may influence the release of adrenaline and cortisol, throwing off hormonal balance and abnormally raising or lowering cortisol levels, leading to sleep disturbances.
Cortisol levels are naturally highest in the morning hours, around 0800, waking us and providing energy for daily activities. Cortisol levels gradually decrease during the day and are usually lowest between 2400 and 0400 hours, allowing for sleep. For those experiencing acute or chronic stressors, cortisol levels may be raised in the evening, making restful sleep difficult and possibly fragmented. When higher levels of cortisol are sustained, the body accommodates them and needs to continually produce more and more cortisol, eventually depleting cortisol stores along with the body’s ability to regulate the timing of its release. If you wake at 0200 hours and can’t get back to sleep, it could be that your cortisol production began early to try to fulfill your body’s already depleted 24-hour need.
The problem can become circular: If you experience abnormally high levels of cortisol in the evening, your ability to fall asleep will be disrupted. If you experience abnormally low cortisol levels throughout the day, your body may work overtime to raise cortisol levels. If you lose sleep for even one night, your body’s normal stress response may accelerate cortisol release, throwing cortisol levels off balance. This can then affect your body’s metabolic processes and human cognition. Needless to say, regular exercise and relaxation activities, anything you can do to maintain health and reduce stressors, will help alleviate sleep disturbances and improve alertness.
- “Let’s grab some fast food and call it a night.” Nutrition is often overlooked as a contributing factor to fatigue and fatigue prevention. Maintaining a balanced diet of high protein, low fat, and low simple sugar carbohydrates and eating at regular intervals, including not skipping breakfast, will help the body maintain energy levels and fight fatigue. Consider carrying healthy snacks to provide an easily available energy boost when you start to feel tired or hungry between meals. Also, avoid large meals before bedtime, as digestion is controlled by the circadian rhythm and naturally slows from 0100-0500 hours daily. This doesn’t mean you should go to bed hungry; a small, light meal or snack consisting of foods high in tryptophan2 (e.g., turkey, soy, warm milk) may aid relaxation and contribute to a more restful sleep.
Much has been written about proper hydration in the recovery and rehabilitation of firefighters, but drinking fluids throughout the day is also necessary to increase alertness. Dehydration can increase sluggishness, irritability, and headaches and make it more difficult to maintain concentration, including the ability to perform simple math, visually track, and use short-term memory effectively. That said, you must coordinate hydration with other bodily processes, including elimination processes and sleep cycles. Consider reducing fluid intake before bed to minimize the number of trips to the bathroom during what should be sleep time.
Maintaining Alertness
Firefighters have come up with numerous ways to maintain alertness on the job. However, some of the methods developed to circumvent sleepiness or promote alertness may be aggravating the problem rather than correcting it. Below are a few of the more common alertness remedies employed in the firehouse, along with guidance on how to adapt these methods so you can properly achieve adequate, healthy results.
- “I’ve mastered the open-eyed nap.” Napping can be used to supplement too little or poor quality sleep, but you must plan a nap to gain the most benefit from it and reduce the chance that it will prevent you from falling asleep and achieving a good night of rest. Consider taking a nap if the last sleep period included <six hours of sleep, if you have experienced multiple periods of wakefulness during a regular sleep cycle, or if you are unusually tired or lethargic and are drifting in and out of sleep. Determine the duration of the nap by the amount of sleep lost. If possible, keep the nap to under an hour; longer naps may interfere with subsequent sleep and it may be difficult to wake up because the body may enter deeper sleep cycles. Allow 15-20 minutes to recover from sleep inertia (grogginess) before operating a vehicle or performing safety critical tasks.3

If at all possible, take a nap during the times of circadian low, when the body is naturally more tired, such as in the afternoon. Considering a routine daytime roster, morning-personality types would ideally nap around 1300 or 1330 hours; evening-personality types might want to wait until 1430 or 1500 hours. As a general rule, avoid napping in the morning, when the body naturally encounters circadian spikes of wakefulness, especially from 1000-1200 hours. There are, of course, exceptions to this rule of thumb – for example, if you lost a considerable amount of sleep immediately prior to a duty day, taking a nap longer than an hour prior to going on shift and as close to the beginning of the shift as possible will prove beneficial. When time allows, a 10- to 15-minute “power nap” can provide a substantial boost in alertness but only for short periods of time. Naps are a good strategy for increasing alertness, but they do not replace adequate restorative sleep.
- “Doc said sleep is good. I’ll sleep in the recliner while the news is on.” Just as important as when and how long to sleep is where to sleep. The recliner in front of the television or anywhere other distractions and interruptions exist does not afford restorative rest. Noise, lighting, and even smells can stimulate the brain, which craves sensory input and continues to take in sensory cues from the environment throughout sleep. During sleep, though, the brain does not consciously manage attention given to these sensory cues as it does during periods of wakefulness. These unfiltered sensory cues may provide enough stimulation to disturb sleep by arousing the brain and increasing heart rate and blood pressure, causing you to move, shift between sleep stages, or even fully awaken. Some people are more sensitive to noise than others. Although the brain can adapt to some low levels of ambient background noise, random or peak noises will disrupt sleep. In a sleep study that considered the combined effects of noise on recuperative sleep, scientists discovered that people attuned to noise in the environment (demonstrated by fewer brain wave changes) when exposed to noise on 11 consecutive nights. Interestingly, their cardiac arousals (demonstrated by heart rate) did not acclimatize.
A controlled environment promotes healthy sleep. This means retreating to a protected area where the lights can be turned off or blacked out entirely, noise is reduced, and cooler temperatures are maintained. This downtime area must be safeguarded by policy as much as possible. If it’s impossible to dampen all stimuli, consider noise-cancelling ear buds or a white noise device. Scientific evidence suggests that low-level white noise, such as gentle rain, a whirring fan, or a sound machine, provides a harmonic signal that dampens the brain’s internal activity.
- “Just give me a cup of coffee, and I’m good to go.” As on many job sites, there’s always caffeine in a firehouse. Who doesn’t know that person who carries a cup of coffee in his hand throughout the day? Caffeine’s effects are temporary and vary by individual. It takes roughly 15-30 minutes before a person may experience the effects of caffeine, and they may last four hours or more. Regular or excessive use can lead to caffeine tolerance, wherein caffeine will cease to increase energy and alertness. Caffeine can be habit forming, and when more than ~250 mgs of caffeine are consumed per day, people may suffer caffeine side effects that result in losing even more sleep. Caffeine must be used judiciously and only as a tool to increase alertness and performance. Caffeine masks fatigue; it doesn’t eliminate it.
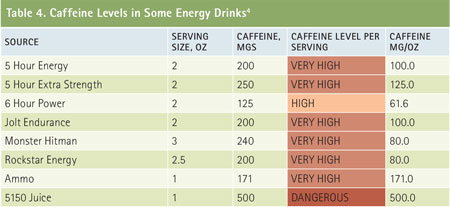
How much caffeine is in that coffee anyway? Tables 3-5 reflect the caffeine levels in some popular beverages. Ratings are based on a diet consisting of 250 mgs or less of caffeine consumption per day.
Many energy shots, sodas, and tea drinks contain amounts of sugar that give short bursts of energy and a subsequent blood sugar crash. If nursing a hot cup of coffee is a habit that’s hard to break, the benefits of switching to decaffeinated coffee or tea cannot be overstated.
Sleep Is the Only Cure
The most important takeaway point from this article is that you should not lose sight of what you do in your off-duty time. At the very least, stick to a regular sleep schedule that affords solid, consistent sleep on off-duty days. A soothing routine before bedtime, such as a warm shower, meditation, or reading a book, will help promote sleep. Follow the restorative sleep period with activities that promote alertness such as exposure to light, exercise, or outdoor activities.
Consider mapping your sleep habits using a commonly available fitness tracking device or an app. Recording sleep/wake patterns can provide valuable insight into good and poor sleep habits and may alert you to disruptions that occur when you are asleep.
Losing sleep is much more than living in a fatigued state; it can also damage your long-term health and increase vulnerability for a cardiovascular event. Understanding how habits help or harm sleep patterns and making lifestyle adjustments will allow you to maintain not only fitness for duty but also fitness for life. If it comes down to getting to sleep on time or waking on time, it’s best to maintain the same wake time. So, when catching up on your sleep, be sure to get to bed early.
Endnotes
1. The intent of this article is to promote awareness of the health issues and provide insight into culturally accepted norms associated with fatigue. Given the variation in work policy and scheduling among the readership, it may not be prudent to provide overly prescriptive guidelines as a one-size-fits-all approach.
2. Because of tryptophan’s ability to raise serotonin levels, which helps the body regulate hunger, sleep, and mood, tryptophan is used to treat of a variety of conditions such as insomnia, depression, and anxiety.
3. Although this is ideal, an active alarm can provide enough stimulus to raise adrenaline levels to shake off grogginess.
4. Caffeine levels derived from http://www.caffeineinformer.com and represent averages.
Bibliography
Alvarez, D, Hornero, R, Marcos, J V, & Campo, F. (2010) “Multivariate analysis of blood oxygen saturation recordings in obstructive sleep apnea diagnosis,” Biomedical Engineering, IEEE Transactions on; 57(12), 2816-2824.
Basner, M, Müller, U, & Elmenhorst, EM. (2011). “Single and Combined Effects of Air, Road, and Rail Traffic Noise on Sleep and Recuperation,” Sleep; 34(1), 11-23.
Hoevenaar-Blom, MP, Spijkerman, AM, Kromhout, D, & Verschuren, WM (2014). “Sufficient sleep duration contributes to lower cardiovascular disease risk in addition to four traditional lifestyle factors: the MORGEN study.” European Journal of Preventive Cardiology; 21(11), 1367-1375.
Punjabi, NM. (2008). The epidemiology of adult obstructive sleep apnea, Proceedings of the American Thoracic Society; 5(2), 136-143.
Sofi, F, Cesari, F, Casini, A, Macchi, C, Abbate, R, & Gensini, GF. (2014). “Insomnia and risk of cardiovascular disease: a meta-analysis,” European Journal of Preventive Cardiology; 21(1), 57-64.
Van Cauter, E, Spiegel, K, Tasali, E, & Leproult, R. (2008). “Metabolic consequences of sleep and sleep loss,” Sleep medicine; 9, S23-S28.
TERRY L. VON THADEN, Ph.D., is a human factors scientist at the University of Illinois Fire Service Institute, with faculty appointments in industrial and enterprise systems engineering, and psychology. Her research involves accident investigation and distributed information practice in safety and time-critical environments including first response, aviation, medical, nuclear, security, military, and transportation operations. She has developed tools and methods used to benchmark and longitudinally track safety culture and decision making in more than 250 organizations in these industries. She serves on numerous government-industry working groups and editorial boards and maintains numerous academic society memberships. She serves as an expert for the Government Accountability Office and National Academy of Sciences-appointed committees on safety issues; she has developed maintenance Fatigue Risk Management guidelines for the Federal Aviation Administration.
Disrupted Sleep and Safety on Scene
Sleep Deprivation in EMS
SLEEP TO SURVIVE: HOW TO MANAGE SLEEP DEPRIVATION
Fire Engineering Archives

