BY KATHERINE WEST
Since the time of HippoCRATES, the first responsibility of health care has been to provide good patient care. Hippocrates’ creed, “Primum non nocerum,” (First, do no harm) has guided health care providers for centuries.1 Over time and with the onset of new diseases, a shift has occurred: Concern for health care worker (HCW) safety has become the primary focus and concern; patient safety has taken a back seat. It is time to put patients at the top of our list of priorities, along with care providers. All too often, the safety risks to health care workers are overstated, leading to poor patient care. Providing optimal care requires simultaneously addressing the safety needs of both the HCW and the patient.
The need for balance is most evident during the influenza season. Coupled with the documented rise in common childhood diseases that have returned, HCWs today have the opportunity to be exposed to many airborne or droplet-transmitted diseases. Additional attention must be directed toward disease prevention and limiting HCW exposure to these diseases. The risks associated with influenza and childhood diseases are known, and preventive vaccines are available. There appears to be a “disconnect” regarding acceptance of vaccines offered to HCWs and their professed concern for illnesses acquired at work. Many HCWs refuse vaccines that are known to protect them. This puts them at risk and increases risk to the patients they serve. Why do HCWs resist being vaccinated?
If an office worker becomes ill, the illness may spread to coworkers sitting in close proximity. When ill HCWs report to work, they affect not only coworkers but also all of the patients they see. Some of those patients may already have conditions that make them more susceptible to infection. The ill HCW also has a lowered immune response, which makes him more susceptible as well. In the fire/EMS community, there is great concern expressed for protecting family members, yet many EMS workers decline protective vaccines (such as the flu vaccine) that would also serve to protect their families. HCWs are also often reluctant to provide health information that would identify their need for protective vaccines. This seems illogical and may be caused by a lack of understanding the science behind vaccine/immunization recommendations. Another statement of Hippocrates was, “There are in fact, two things: science and opinion; the former begets knowledge; the latter ignorance.” (1)
In 2010 at the Cleveland Clinic Children’s Hospital, an HCW worked for 22 days with an atypical “barky” cough that was eventually diagnosed as pertussis (whooping cough). Since she declined to receive the recommended booster of Tdap (tetanus, diphtheria, acelluar pertussis), the employee exposed 23 pediatric patients in the hematology-oncology ward as well as 31 other infants and 92 coworkers. Cleveland Clinic has a comprehensive HCW vaccination program, yet a review following this outbreak revealed that only 43 percent of the exposed HCWs had accepted the vaccine.2
This is a clear example of a disconnect: HCWs declining vaccination and placing high-risk pediatric patients at risk for a disease (pertussis) that has returned in large numbers in the United States. The Centers for Disease Control and Prevention (CDC) identified more than 41,000 cases of pertussis in 2012. This exceeds reported bloodborne pathogen cases. Of note, CDC first recommended pertussis boosters for HCWs in 2006 and reiterated this in 2011. (2)
Curiously, few EMS agencies seemed aware of this recommendation, and most occupational medicine practices did not advise their EMS clients of this. It is vital for departments to stay abreast of new vaccine/immunization recommendations. They serve department members well since their personal health maintenance protects patients, them, and their family members. In an interview for the PBS News Hour in 2012, the head of the American Nurses Association noted: “HCW vaccination is an ‘ethical responsibility’; part of the nursing’s code of ethics is that the patient comes first.”
Does not fire/EMS have the same “duty to care”? The EMS Educational Standards, outlined in EMT textbooks, clearly state, “Without question, our first duty as EMS providers is to do no further harm to a patient.” The Standards also note, “You have a duty to maintain your health and psychological well-being.”3
So why do HCWs decline vaccines? Perhaps it is centered on concerns for the safety and efficacy of vaccines. Earlier vaccines were egg-based, and allergy was an issue for some people. Current vaccines contain live virus to enhance immune response that often mimics natural infection. This leads some to believe that the vaccine causes the flu. Actually, it is the vaccine working for the individual; the immune response is so considerably less than natural infections that most people barely notice it. In contrast, killed virus vaccines often have limited effectiveness. However, times are changing: Newer DNA vaccines do not contain virus components at all.4 This is the future for all vaccines.
Education is the key to understanding the science and the benefits of vaccination. This is an important part of “informed consent.” During the H1N1 pandemic in 2009, approximately 37 percent of HCWs received preventive vaccines. In three published studies looking at EMS participation in influenza vaccine programs, the reported participation rate was 21 percent, and 48 percent for U.S. EMTs. This was a far lower rate than for other U.S. health care groups.5
In today’s world, the newest vaccines are not egg-based; they are DNA based. In DNA-based vaccines, the direct injection of genetic material into a living host causes a small amount of its cells to produce the introduced gene products. The host (i.e., the HCW) customizes the vaccine. This results in the specific immune activation of the host HCW against the gene-delivered antigen. This is believed to enhance antibody response. DNA vaccines allow for rapid and large-scale production and cost considerably less than traditional vaccines. DNA-based vaccines are also very temperature stable, making storage and transport much easier. These vaccines can also be altered quickly should a change in the vaccine makeup be needed for evolving disease patterns.
On January 16, 2013, the U.S. Food and Drug Administration approved a new DNA flu vaccine, sold under the name Flublok. Science and research are leading the way for changes in all vaccines. Perhaps the availability of this vaccine, as well as other DNA-based vaccines, will improve vaccine participation rates.6
MANDATING INFLUENZA VACCINE
Hippocrates also told us, “Extreme remedies are very appropriate for extreme diseases.” Many HCWs do not realize that influenza and childhood diseases can lead to death. In 2010, 10 children in California died of pertussis, a preventable disease. In the United States, at least 30,000 to 40,000 people die each year from seasonal influenza. In addition, at least 300,000 are hospitalized with seasonal influenza, and the costs associated with these admissions continue to climb. Medical facilities across the country are making influenza vaccination a “condition of employment,” allowing declination only for medical exemption. HCWs with medical exemption need to wear surgical masks during their entire work shift. In many facilities, EMS workers are being asked to wear surgical masks when entering medical facilities if they are unvaccinated. HCWs have an annual influenza infection rate of 18.7 percent. Unvaccinated HCWs have a 24 percent infection rate, an incidence seen only in unvaccinated adults living with children.
Some states and local governments have passed laws requiring certain groups to receive influenza vaccination. They include schoolchildren, military personnel, and HCWs. California passed a hospital influenza law requiring facilities to offer free vaccine with “required” participation and mandatory use of a declination form.7
The first large hospital to mandate flu vaccine for staff was Virginia Mason Medical Center in Seattle, Washington, in 2005-06. The annual participation rate in this facility had been about 44 percent; after the mandate, it rose to 98 percent. (7)
Many medical organizations have published position papers calling for the development and implementation of a mandatory influenza vaccination policy at medical facilities. They include the American Academy of Pediatrics, Infectious Disease Society of America, American Hospital Association, American Medical Directors Association, American Public Health Association, Association for Professionals in Infection Control and Epidemiology, American Nurses Association, and many more. The Immunization Action Coalition publishes an extensive listing.8 The Joint Commission on Accreditation of Healthcare Organizations (TJC) standard views this as a patient safety measure.
The Occupational Safety and Health Administration (OSHA) noted in a letter of written opinion, “OSHA does not require that an employee take a vaccine, but an employer may do so.”9 On a federal level, the National Vaccine Advisory Committee (NVAC) is working on a draft document to the Department of Health and Human Services stating that medical facilities failing to reach a 90 percent immunization level should strongly consider an employer requirement for influenza immunization. (9)
DECLINATION FORMS
Declination forms were first introduced by OSHA for its Hepatitis B vaccine program requirements in the Bloodborne Pathogens Regulation, 29 CFR 1910.1030. A requirement for declination forms also is contained in CDC guidelines and National Fire Protection Association (NFPA) 1581, Standard on Fire Department Infection Control Program.
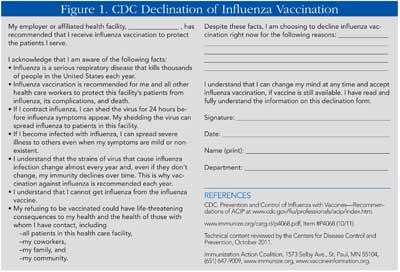
The use of declination forms has a twofold rationale and is part of all vaccine/immunization programs. Declination forms not only document that the employer met its obligation to offer the vaccines/immunizations but also ensure that the employee is fully informed about any misconceptions, risks, and the importance of promoting patient safety (Figure 1).10 Declination forms are needed for all the recommended vaccines for fire/EMS providers. Currently, the vaccines required to be offered to nonprotected personnel include hepatitis B vaccine, Tdap booster, measles, mumps, rubella vaccine, chickenpox vaccine, and seasonal flu vaccine; tuberculosis testing is also required.
Declination forms do not remove any right to sick time or workers’ compensation coverage if an employee develops a preventable illness. However, many risk managers in medical facilities today prohibit students from doing clinical rotations for EMS training if they have signed declination forms. Facilities see this as a risk management issue. Remember, with regard to seasonal flu, medical facilities may require that unvaccinated EMS personnel wear a surgical mask on entering their facility.11 Vaccine programs also protect you (the care provider); when you are protected, you will not take the flu or other droplet-transmitted diseases home to your family.
COST ISSUES
The cost of the vaccine is often raised by department administration as an objection to having vaccine programs. This thinking is considerably off base. Vaccination programs are actually a cost-saving measure. For example, in the Cleveland Clinic pertussis case, the costs for medical follow-up of exposed personnel and patients, lost work time, and medical referrals came to about $12,065. The cost to vaccinate a HCW was $30. In the case of influenza, consider the number of employees calling in sick for three to five days at a clip vs. the cost of a flu shot! The cost of vaccination vs. sick time and postexposure follow-up is very easy math. (2)
WORK RESTRICTION GUIDELINES
In 1997, the CDC published work restriction guidelines, which listed various illnesses and whether or not a health care worker should or should not be at work. These guidelines were updated on November 25, 2011, in the “Immunizations for Health Care Personnel Guidelines.” They are practical and help protect both HCWs and patients. They should be department policy, included in the Exposure Control Plan, and reviewed in staff education and training.
Here again, however, a “disconnect” becomes evident. For example, an EMS provider may worry about contracting a bloodborne pathogen illness and yet come to work with open poison-ivy lesions on both arms with plenty of potential for a nonintact skin/blood exposure. The CDC, OSHA, and NFPA all require HCWs with nonintact skin to have the areas covered with a dressing. If the areas are too large, the provider is restricted from doing patient care. This is often ignored in fire and EMS departments. CDC guidelines call for HCWs with seasonal influenza/upper respiratory infections to be excluded from duty until 24 hours after being fever free (without the use of fever-reducing medicines such as acetaminophen). (11)
Yet, work restriction is often not addressed in policy, training, or compliance monitoring. There are two important issues here. The first is reducing risk for infection in the ill care provider. Working when ill becomes an issue because the individual’s immune system is weakened and perhaps more susceptible to infection. Second, there is an issue of potential liability if a patient acquires an illness from the HCW. This has become a bigger issue as medical facilities are no longer reimbursed by the Centers for Medicare and Medicaid Services for costs associated with hospital-acquired infections. If a facility can establish that the acquired infection was the fault of EMS and not the medical facility, a lawsuit may follow-not only from the patient who acquired the infection but also possibly from the medical facility for lost reimbursed funds.
BATTLE WILL CONTINUE
It appears that until HCW participation rates increase, the battle between concerns about vaccine safety vs. protecting EMS providers and patients will continue. What is clear and, unfortunately, may require legislative intervention to accomplish, is that vaccination serves the best interests of fire and EMS providers as well as the patients we serve. After all, we do see and care for sick people every day.
References
1. Hippocrates, Quotes.
2. Gagliano, Gregory, “A healthcare worker with pertussis: High cost and lost opportunity,” Prevention strategist, Winter, 2012,5(4):50-53.
3. Caroline, Nancy. Emergency Care in the Streets, Sixth Edition. Jones and Bartlett Publishers; 2008:4.10.
4. “New DNA Vaccine Technology Poised to Deliver Safe and Cost-effective Disease Protection,” Science Daily, November 12, 2012.
5. Terri Rebmann, Kathleen Wright, et al, “Seasonal and H1N1 influenza vaccine compliance and the intent to be vaccinated among emergency medical services personnel,” Am. Journal of Infection Control, September 2012;40(7):632-636.
6. FDA Press Release, Flubok, January 13, 2012.
7. California Hospital Influenza Law, SB 739, California Health and Safety Code, January 1, 2007.
8. First Do No Harm: Mandatory Influenza Vaccination Policies for Healthcare Personnel (HCP) Help Project Patients, Immunization Action Coalition, St. Paul, Minnesota.
9. OSHA Letter of Interpretation, 2009.
10. Talbot, Thomas, “Do Declination Statements Increase Health Care Worker Influenza Vaccination Rates?” Clinical Infectious Diseases, 2009;49(5):773-779.
11. “Immunization of Healthcare Personnel,” MMWR, Centers for Disease Control and Prevention, November 25, 2011.
● KATHERINE WEST, BSN, MSEd, is an infection control consultant actively working with fire and EMS since 1978. She lectures nationally and internationally and has authored books, videos, and articles on infection-control issues. She has served as a consultant to the Centers for Disease Control and Prevention and the National Institute for Occupational Safety and Health and as an education specialist for the National Institutes of Health. She authored the Infectious Disease Handbook for Emergency Care Personnel, now in its third edition. She is also a consultant to the U.S. Public Health Service and Federal Occupational Health. She received the Association for Professionals in Infection Control & Epidemiology 2006 “Hero in Infection Control & Prevention” award.
More Fire Engineering Issue Articles
Fire Engineering Archives

